Primary Retinal Detachment
Primary Retinal Detachment
Primary Retinal Detachment
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
86<br />
5 Vitrectomy for the <strong>Primary</strong> Management of <strong>Retinal</strong> <strong>Detachment</strong><br />
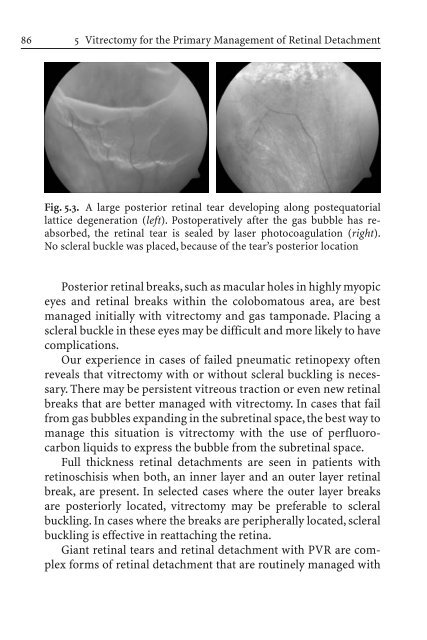
Fig. 5.3. A large posterior retinal tear developing along postequatorial<br />
lattice degeneration (left). Postoperatively after the gas bubble has reabsorbed,<br />
the retinal tear is sealed by laser photocoagulation (right).<br />
No scleral buckle was placed, because of the tear’s posterior location<br />
Posterior retinal breaks, such as macular holes in highly myopic<br />
eyes and retinal breaks within the colobomatous area, are best<br />
managed initially with vitrectomy and gas tamponade. Placing a<br />
scleral buckle in these eyes may be difficult and more likely to have<br />
complications.<br />
Our experience in cases of failed pneumatic retinopexy often<br />
reveals that vitrectomy with or without scleral buckling is necessary.<br />
There may be persistent vitreous traction or even new retinal<br />
breaks that are better managed with vitrectomy. In cases that fail<br />
from gas bubbles expanding in the subretinal space, the best way to<br />
manage this situation is vitrectomy with the use of perfluorocarbon<br />
liquids to express the bubble from the subretinal space.<br />
Full thickness retinal detachments are seen in patients with<br />
retinoschisis when both, an inner layer and an outer layer retinal<br />
break, are present. In selected cases where the outer layer breaks<br />
are posteriorly located, vitrectomy may be preferable to scleral<br />
buckling. In cases where the breaks are peripherally located, scleral<br />
buckling is effective in reattaching the retina.<br />
Giant retinal tears and retinal detachment with PVR are complex<br />
forms of retinal detachment that are routinely managed with