Eble JN, Sauter G., Epstein JI, Sesterhenn IA - iarc
Eble JN, Sauter G., Epstein JI, Sesterhenn IA - iarc
Eble JN, Sauter G., Epstein JI, Sesterhenn IA - iarc
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
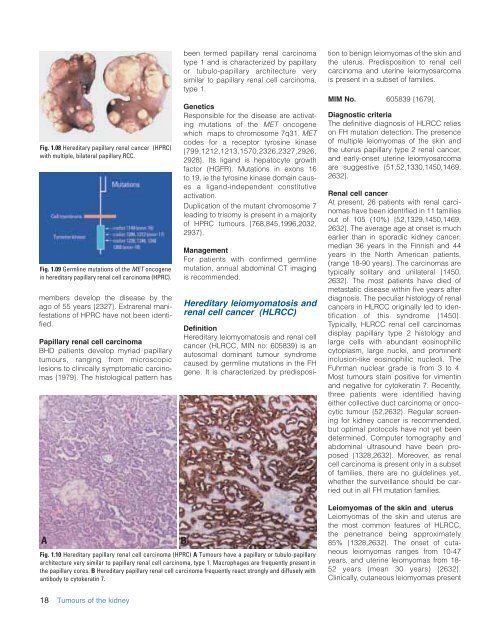
Fig. 1.08 Hereditary papillary renal cancer (HPRC)<br />
with multiple, bilateral papillary RCC.<br />
Fig. 1.09 Germline mutations of the MET oncogene<br />
in hereditary papillary renal cell carcinoma (HPRC).<br />
members develop the disease by the<br />
ago of 55 years {2327}. Extrarenal manifestations<br />
of HPRC have not been identified.<br />
Papillary renal cell carcinoma<br />
BHD patients develop myriad papillary<br />
tumours, ranging from microscopic<br />
lesions to clinically symptomatic carcinomas<br />
{1979}. The histological pattern has<br />
been termed papillary renal carcinoma<br />
type 1 and is characterized by papillary<br />
or tubulo-papillary architecture very<br />
similar to papillary renal cell carcinoma,<br />
type 1.<br />
Genetics<br />
Responsible for the disease are activating<br />
mutations of the MET oncogene<br />
which maps to chromosome 7q31. MET<br />
codes for a receptor tyrosine kinase<br />
{799,1212,1213,1570,2326,2327,2926,<br />
2928}. Its ligand is hepatocyte growth<br />
factor (HGFR). Mutations in exons 16<br />
to 19, ie the tyrosine kinase domain causes<br />
a ligand-independent constitutive<br />
activation.<br />
Duplication of the mutant chromosome 7<br />
leading to trisomy is present in a majority<br />
of HPRC tumours {768,845,1996,2032,<br />
2937}.<br />
Management<br />
For patients with confirmed germline<br />
mutation, annual abdominal CT imaging<br />
is recommended.<br />
Hereditary leiomyomatosis and<br />
renal cell cancer (HLRCC)<br />
Definition<br />
Hereditary leiomyomatosis and renal cell<br />
cancer (HLRCC, MIN no: 605839) is an<br />
autosomal dominant tumour syndrome<br />
caused by germline mutations in the FH<br />
gene. It is characterized by predisposition<br />
to benign leiomyomas of the skin and<br />
the uterus. Predisposition to renal cell<br />
carcinoma and uterine leiomyosarcoma<br />
is present in a subset of families.<br />
MIM No. 605839 {1679}.<br />
Diagnostic criteria<br />
The definitive diagnosis of HLRCC relies<br />
on FH mutation detection. The presence<br />
of multiple leiomyomas of the skin and<br />
the uterus papillary type 2 renal cancer,<br />
and early-onset uterine leiomyosarcoma<br />
are suggestive {51,52,1330,1450,1469,<br />
2632}.<br />
Renal cell cancer<br />
At present, 26 patients with renal carcinomas<br />
have been identified in 11 families<br />
out of 105 (10%) {52,1329,1450,1469,<br />
2632}. The average age at onset is much<br />
earlier than in sporadic kidney cancer;<br />
median 36 years in the Finnish and 44<br />
years in the North American patients,<br />
(range 18-90 years). The carcinomas are<br />
typically solitary and unilateral {1450,<br />
2632}. The most patients have died of<br />
metastatic disease within five years after<br />
diagnosis. The peculiar histology of renal<br />
cancers in HLRCC originally led to identification<br />
of this syndrome {1450}.<br />
Typically, HLRCC renal cell carcinomas<br />
display papillary type 2 histology and<br />
large cells with abundant eosinophilic<br />
cytoplasm, large nuclei, and prominent<br />
inclusion-like eosinophilic nucleoli. The<br />
Fuhrman nuclear grade is from 3 to 4.<br />
Most tumours stain positive for vimentin<br />
and negative for cytokeratin 7. Recently,<br />
three patients were identified having<br />
either collective duct carcinoma or oncocytic<br />
tumour {52,2632}. Regular screening<br />
for kidney cancer is recommended,<br />
but optimal protocols have not yet been<br />
determined. Computer tomography and<br />
abdominal ultrasound have been proposed<br />
{1328,2632}. Moreover, as renal<br />
cell carcinoma is present only in a subset<br />
of families, there are no guidelines yet,<br />
whether the surveillance should be carried<br />
out in all FH mutation families.<br />
A<br />
Fig. 1.10 Hereditary papillary renal cell carcinoma (HPRC) A Tumours have a papillary or tubulo-papillary<br />
architecture very similar to papillary renal cell carcinoma, type 1. Macrophages are frequently present in<br />
the papillary cores. B Hereditary papillary renal cell carcinoma frequently react strongly and diffusely with<br />
antibody to cytokeratin 7.<br />
B<br />
Leiomyomas of the skin and uterus<br />
Leiomyomas of the skin and uterus are<br />
the most common features of HLRCC,<br />
the penetrance being approximately<br />
85% {1328,2632}. The onset of cutaneous<br />
leiomyomas ranges from 10-47<br />
years, and uterine leiomyomas from 18-<br />
52 years (mean 30 years) {2632}.<br />
Clinically, cutaneous leiomyomas present<br />
18<br />
Tumours of the kidney