Eble JN, Sauter G., Epstein JI, Sesterhenn IA - iarc
Eble JN, Sauter G., Epstein JI, Sesterhenn IA - iarc
Eble JN, Sauter G., Epstein JI, Sesterhenn IA - iarc
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
and prostatectomy Gleason score<br />
{375,668,2498}. Exact correlation has<br />
been observed in 28.2-67.9% of the<br />
cases. The biopsies undergraded in 24.5-<br />
60.0% and overgraded in 5.2-32.2%.<br />
Causes for biopsy grading discrepencies<br />
are undersampling of higher or<br />
lower grades, tumours borderline<br />
between two grade patterns, and misinterpretation<br />
of patterns {2498}. The concordance<br />
between biopsy and prostatectomy<br />
Gleason score is within one<br />
Gleason score in more than 90% of<br />
cases {668}.<br />
Reproducibility<br />
Pathologists tend to undergrade<br />
{665,2498}. The vast majority of tumours<br />
graded as Gleason score 2 to 4 on core<br />
biopsy are graded as Gleason score 5 to<br />
6 or higher when reviewed by experts in<br />
urological pathology {2498}. In a recent<br />
study of interobserver reproducibility<br />
amongst general pathologists, the overall<br />
agreement for Gleason score groups<br />
2-4, 5-6, 7, and 8-10 was just into the<br />
moderate range {67}. Undergrading is<br />
decreased with teaching efforts and a<br />
substantial interobserver reproducibility<br />
can be obtained {665,1400}.<br />
Prognosis<br />
Multiple studies have confirmed that<br />
Gleason score is a very powerful prognostic<br />
factor on all prostatic samples.<br />
This includes the prediction of the natural<br />
history of prostate cancer {54,667} and<br />
the assessment of the risk of recurrence<br />
after total prostatectomy {713,1144} or<br />
radiotherapy {937}. Several schedules<br />
for grouping of Gleason scores in prognostic<br />
categories have been proposed.<br />
Gleason scores 2 to 4 behave similarly<br />
and may be grouped. Likewise, Gleason<br />
scores 8 to 10 are usually grouped<br />
together, although they could be stratified<br />
with regard to disease progression in<br />
a large prostatectomy study {1446}.<br />
There is evidence that Gleason score 7 is<br />
a distinct entity with prognosis intermediate<br />
between that of Gleason scores 5-6<br />
and 8 to 10, respectively {667,2590}.<br />
Although the presence and amount of<br />
high grade cancer (patterns 4 to 5) correlates<br />
with tumour prognosis, reporting<br />
the percentage pattern 4/5 is not routine<br />
clinical practice {666,2479}. Gleason<br />
score 7 cancers with a primary pattern 4<br />
have worse prognosis than those with a<br />
primary pattern 3 {406,1447,2282}.<br />
Genetics<br />
In developed countries, prostate cancer<br />
is the most commonly diagnosed nonskin<br />
malignancy in males. It is estimated<br />
that 1 in 9 males will be diagnosed with<br />
prostate cancer during their lifetime.<br />
Multiple factors contribute to the high<br />
incidence and prevalence of prostate<br />
cancer. Risk factors include age, family<br />
history, and race. Environmental exposures<br />
are clearly involved as well.<br />
Although the exact exposures that<br />
increase prostate cancer risk are<br />
unclear, diet (especially those high in<br />
animal fat such as red meat, as well as,<br />
those with low levels of antioxidants such<br />
as selenium and vitamin E) job/industrial<br />
chemicals, sexually transmitted infections,<br />
and chronic prostatitis have been<br />
implicated to varying degrees. The<br />
marked increase in incidence in prostate<br />
cancer that occurred in the mid 1980s,<br />
which subsequently leveled off in the<br />
mid to late 1990s, indicates that wide<br />
spread awareness and serum prostate<br />
specific antigen screening can produce<br />
a transient marked increase in prostate<br />
cancer incidence.<br />
Hereditary prostate cancer<br />
Currently the evidence for a strong<br />
genetic component is compelling.<br />
Observations made in the 1950s by<br />
Morganti and colleagues suggested a<br />
strong familial predisposition for prostate<br />
cancer {1784}. Strengthening the genetic<br />
evidence is a high frequency for prostate<br />
cancer in monozygotic as compared to<br />
dizygotic twins in a study of twins from<br />
Sweden, Denmark, and Finland {1496}.<br />
Work over the past decade using<br />
genome wide scans in prostate cancer<br />
families has identified high risk alleles,<br />
displaying either an autosomal dominant<br />
or X-linked mode of inheritance for a<br />
hereditary prostate cancer gene, from at<br />
least 7 candidate genetic loci. Of these<br />
loci, three candidate genes have been<br />
identified HPC2/ELAC2 on 17p {2584},<br />
RNASEL on 1q25 {377}, and MSR1 on<br />
8p22-23 {2857}. These 3 genes do not<br />
account for the majority of hereditary<br />
prostate cancer cases. In addition, more<br />
than 10 other loci have been implicated<br />
by at least some groups. The discovery<br />
of highly penetrant prostate cancer<br />
genes has been particularly difficult for at<br />
least 2 main reasons. First, due to the<br />
advanced age of onset (median 60<br />
years), identification of more than two<br />
generations to perform molecular studies<br />
on is difficult. Second, given the high frequency<br />
of prostate cancer, it is likely that<br />
cases considered to be hereditary during<br />
segregation studies actually repre-<br />
A<br />
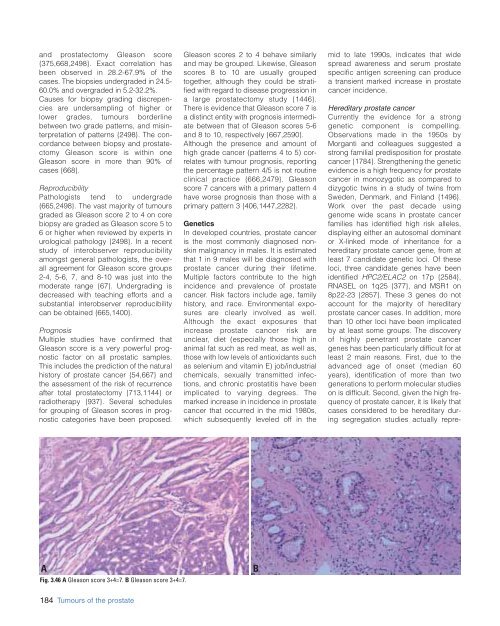
Fig. 3.46 A Gleason score 3+4=7. B Gleason score 3+4=7.<br />
B<br />
184 Tumours of the prostate