Clinical Manual for Management of the HIV-Infected ... - myCME.com
Clinical Manual for Management of the HIV-Infected ... - myCME.com
Clinical Manual for Management of the HIV-Infected ... - myCME.com
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
4–6 | <strong>Clinical</strong> <strong>Manual</strong> <strong>for</strong> <strong>Management</strong> <strong>of</strong> <strong>the</strong> <strong>HIV</strong>-<strong>Infected</strong> Adult/2006<br />
♦<br />
♦<br />
♦<br />
♦<br />
Assess <strong>for</strong> CHD or CHD equivalents.<br />
♦<br />
♦<br />
CHD includes a history <strong>of</strong> myocardial<br />
infarction, unstable angina, stable angina, CHD<br />
procedures, or evidence <strong>of</strong> clinically significant<br />
myocardial ischemia.<br />
CHD equivalents include diabetes, peripheral<br />
vascular disease, carotid artery disease,<br />
abdominal aortic aneurysm, transient ischemic<br />
attacks, or 2 or more CHD risk factors with a<br />
10-year risk <strong>of</strong> CHD >20% (see “Calculations<br />
to Estimate <strong>the</strong> 10-Year Risk <strong>of</strong> Cardiac Events<br />
<strong>for</strong> Men and Women”, below, or <strong>the</strong> online risk<br />
calculator at http://hin.nhlbi.nih.gov/atpiii/<br />
calculator.asp?usertype=pr<strong>of</strong>).<br />
Assess CHD risks. Major risk factors include<br />
hypertension, diabetes, smoking, low HDL, age,<br />
and family history <strong>of</strong> CHD.<br />
Assess <strong>for</strong> causes <strong>of</strong> secondary dyslipidemias,<br />
including diabetes, hypothyroidism, obstructive<br />
liver diseases, chronic renal failure, and medications<br />
such as corticosteroids or progestins.<br />
Screen <strong>for</strong> o<strong>the</strong>r factors that contribute to<br />
hyperlipidemia, including obesity, chronic<br />
liver diseases, alcohol abuse, high-fat or highcarbohydrate<br />
diet, and prothrombotic or<br />
proinflammatory states.<br />
Screen <strong>for</strong> health behaviors that increase CHD risk,<br />
including smoking, high-fat diet, sedentary lifestyle,<br />
and use <strong>of</strong> recreational drugs such as cocaine or<br />
methamphetamine.<br />
Review <strong>the</strong> patient’s family history <strong>for</strong> premature<br />
CHD, obesity, diabetes, and lipid abnormalities.<br />
Review <strong>the</strong> patient’s medications, with special<br />
attention to ARVs known to increase LDL or TG<br />
levels (particularly ritonavir and ritonavir-boosted<br />
PIs) or decrease HDL.<br />
O: Objective<br />
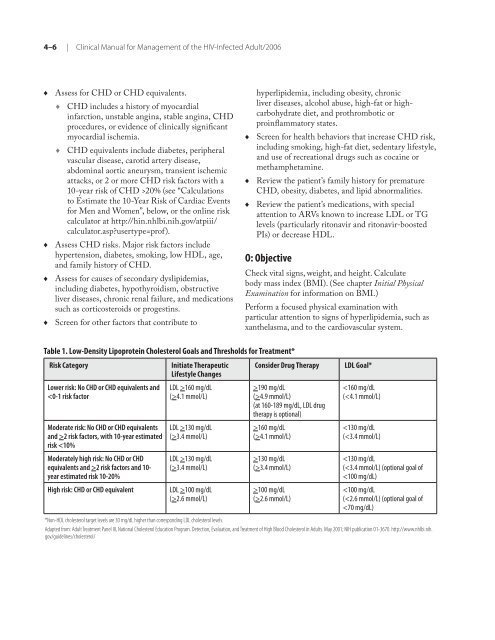
Table 1. Low-Density Lipoprotein Cholesterol Goals and Thresholds <strong>for</strong> Treatment*<br />
Risk Category Initiate Therapeutic<br />
Lifestyle Changes<br />
Lower risk: No CHD or CHD equivalents and<br />
2 risk factors, with 10-year estimated<br />
risk 2 risk factors and 10year<br />
estimated risk 10-20%<br />
LDL >160 mg/dL<br />
(>4.1 mmol/L)<br />
LDL >130 mg/dL<br />
(>3.4 mmol/L)<br />
LDL >130 mg/dL<br />
(>3.4 mmol/L)<br />
High risk: CHD or CHD equivalent LDL >100 mg/dL<br />
(>2.6 mmol/L)<br />
♦<br />
♦<br />
♦<br />
Check vital signs, weight, and height. Calculate<br />
body mass index (BMI). (See chapter Initial Physical<br />
Examination <strong>for</strong> in<strong>for</strong>mation on BMI.)<br />
Per<strong>for</strong>m a focused physical examination with<br />
particular attention to signs <strong>of</strong> hyperlipidemia, such as<br />
xan<strong>the</strong>lasma, and to <strong>the</strong> cardiovascular system.<br />
Consider Drug Therapy LDL Goal*<br />
>190 mg/dL<br />
(>4.9 mmol/L)<br />
(at 160-189 mg/dL, LDL drug<br />
<strong>the</strong>rapy is optional)<br />
>160 mg/dL<br />
(>4.1 mmol/L)<br />
>130 mg/dL<br />
(>3.4 mmol/L)<br />
>100 mg/dL<br />
(>2.6 mmol/L)<br />