Clinical Manual for Management of the HIV-Infected ... - myCME.com
Clinical Manual for Management of the HIV-Infected ... - myCME.com
Clinical Manual for Management of the HIV-Infected ... - myCME.com
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Nonoccupational Postexposure Prophylaxis<br />
Background<br />
Although avoiding exposure to <strong>HIV</strong> is <strong>the</strong> only<br />
reliable way <strong>of</strong> preventing <strong>HIV</strong> infection, postexposure<br />
prophylaxis (PEP) can decrease <strong>the</strong> risk <strong>of</strong> infection<br />
after exposure to <strong>HIV</strong>. Antiretroviral (ARV) <strong>the</strong>rapy is<br />
an important prophylactic intervention in appropriate<br />
persons with nonoccupational exposures (eg, sexual<br />
contact; sharing <strong>of</strong> injection drug needles or o<strong>the</strong>r<br />
equipment), as well as those with occupational<br />
exposures (eg, needlesticks). The U.S. Department<br />
<strong>of</strong> Health and Human Services has established<br />
guidelines <strong>for</strong> nonoccupational PEP (nPEP) based on<br />
data from animal models, perinatal clinical trials, and<br />
observational studies.<br />
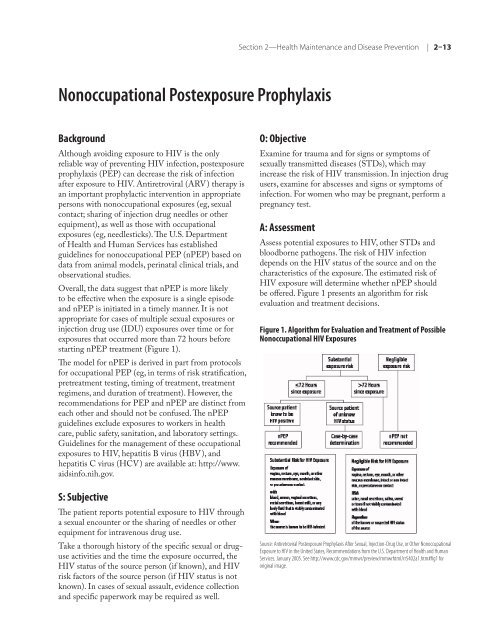
Overall, <strong>the</strong> data suggest that nPEP is more likely<br />
to be effective when <strong>the</strong> exposure is a single episode<br />
and nPEP is initiated in a timely manner. It is not<br />
appropriate <strong>for</strong> cases <strong>of</strong> multiple sexual exposures or<br />
injection drug use (IDU) exposures over time or <strong>for</strong><br />
exposures that occurred more than 72 hours be<strong>for</strong>e<br />
starting nPEP treatment (Figure 1).<br />
The model <strong>for</strong> nPEP is derived in part from protocols<br />
<strong>for</strong> occupational PEP (eg, in terms <strong>of</strong> risk stratification,<br />
pretreatment testing, timing <strong>of</strong> treatment, treatment<br />
regimens, and duration <strong>of</strong> treatment). However, <strong>the</strong><br />
re<strong>com</strong>mendations <strong>for</strong> PEP and nPEP are distinct from<br />
each o<strong>the</strong>r and should not be confused. The nPEP<br />
guidelines exclude exposures to workers in health<br />
care, public safety, sanitation, and laboratory settings.<br />
Guidelines <strong>for</strong> <strong>the</strong> management <strong>of</strong> <strong>the</strong>se occupational<br />
exposures to <strong>HIV</strong>, hepatitis B virus (HBV), and<br />
hepatitis C virus (HCV) are available at: http://www.<br />
aidsinfo.nih.gov.<br />
S: Subjective<br />
The patient reports potential exposure to <strong>HIV</strong> through<br />
a sexual encounter or <strong>the</strong> sharing <strong>of</strong> needles or o<strong>the</strong>r<br />
equipment <strong>for</strong> intravenous drug use.<br />
Take a thorough history <strong>of</strong> <strong>the</strong> specific sexual or druguse<br />
activities and <strong>the</strong> time <strong>the</strong> exposure occurred, <strong>the</strong><br />
<strong>HIV</strong> status <strong>of</strong> <strong>the</strong> source person (if known), and <strong>HIV</strong><br />
risk factors <strong>of</strong> <strong>the</strong> source person (if <strong>HIV</strong> status is not<br />
known). In cases <strong>of</strong> sexual assault, evidence collection<br />
and specific paperwork may be required as well.<br />
Section 2—Health Maintenance and Disease Prevention | 2–13<br />
O: Objective<br />
Examine <strong>for</strong> trauma and <strong>for</strong> signs or symptoms <strong>of</strong><br />
sexually transmitted diseases (STDs), which may<br />
increase <strong>the</strong> risk <strong>of</strong> <strong>HIV</strong> transmission. In injection drug<br />
users, examine <strong>for</strong> abscesses and signs or symptoms <strong>of</strong><br />
infection. For women who may be pregnant, per<strong>for</strong>m a<br />
pregnancy test.<br />
A: Assessment<br />
Assess potential exposures to <strong>HIV</strong>, o<strong>the</strong>r STDs and<br />
bloodborne pathogens. The risk <strong>of</strong> <strong>HIV</strong> infection<br />
depends on <strong>the</strong> <strong>HIV</strong> status <strong>of</strong> <strong>the</strong> source and on <strong>the</strong><br />
characteristics <strong>of</strong> <strong>the</strong> exposure. The estimated risk <strong>of</strong><br />
<strong>HIV</strong> exposure will determine whe<strong>the</strong>r nPEP should<br />
be <strong>of</strong>fered. Figure 1 presents an algorithm <strong>for</strong> risk<br />
evaluation and treatment decisions.<br />
Figure 1. Algorithm <strong>for</strong> Evaluation and Treatment <strong>of</strong> Possible<br />
Nonoccupational <strong>HIV</strong> Exposures<br />
Source: Antiretroviral Postexposure Prophylaxis After Sexual, Injection-Drug Use, or O<strong>the</strong>r Nonoccupational<br />
Exposure to <strong>HIV</strong> in <strong>the</strong> United States, Re<strong>com</strong>mendations from <strong>the</strong> U.S. Department <strong>of</strong> Health and Human<br />
Services. January 2005. See http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5402a1.htm#fig1 <strong>for</strong><br />
original image.