Clinical Manual for Management of the HIV-Infected ... - myCME.com
Clinical Manual for Management of the HIV-Infected ... - myCME.com
Clinical Manual for Management of the HIV-Infected ... - myCME.com
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
5–30 | <strong>Clinical</strong> <strong>Manual</strong> <strong>for</strong> <strong>Management</strong> <strong>of</strong> <strong>the</strong> <strong>HIV</strong>-<strong>Infected</strong> Adult/2006<br />
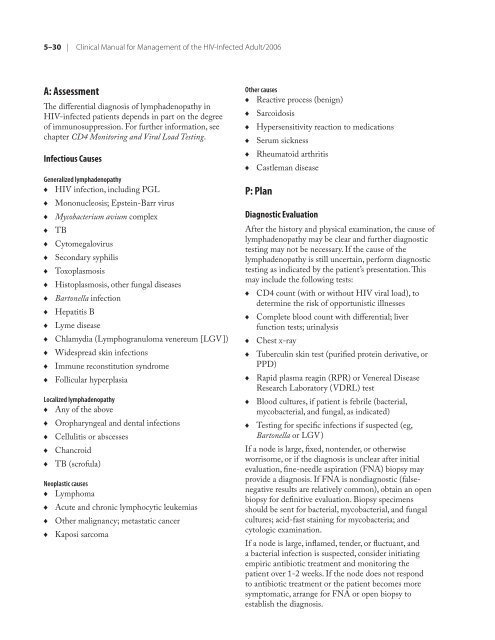
A: Assessment<br />
The differential diagnosis <strong>of</strong> lymphadenopathy in<br />
<strong>HIV</strong>-infected patients depends in part on <strong>the</strong> degree<br />
<strong>of</strong> immunosuppression. For fur<strong>the</strong>r in<strong>for</strong>mation, see<br />
chapter CD4 Monitoring and Viral Load Testing.<br />
Infectious Causes<br />
Generalized lymphadenopathy<br />
♦ <strong>HIV</strong> infection, including PGL<br />
♦<br />
♦<br />
♦<br />
♦<br />
♦<br />
♦<br />
♦<br />
♦<br />
♦<br />
♦<br />
♦<br />
♦<br />
♦<br />
♦<br />
Mononucleosis; Epstein-Barr virus<br />
Mycobacterium avium <strong>com</strong>plex<br />
TB<br />
Cytomegalovirus<br />
Secondary syphilis<br />
Toxoplasmosis<br />
Histoplasmosis, o<strong>the</strong>r fungal diseases<br />
Bartonella infection<br />
Hepatitis B<br />
Lyme disease<br />
Chlamydia (Lymphogranuloma venereum [LGV])<br />
Widespread skin infections<br />
Immune reconstitution syndrome<br />
Follicular hyperplasia<br />
Localized lymphadenopathy<br />
♦ Any <strong>of</strong> <strong>the</strong> above<br />
♦<br />
♦<br />
♦<br />
♦<br />
Oropharyngeal and dental infections<br />
Cellulitis or abscesses<br />
Chancroid<br />
TB (scr<strong>of</strong>ula)<br />
Neoplastic causes<br />
♦ Lymphoma<br />
♦<br />
♦<br />
♦<br />
Acute and chronic lymphocytic leukemias<br />
O<strong>the</strong>r malignancy; metastatic cancer<br />
Kaposi sar<strong>com</strong>a<br />
O<strong>the</strong>r causes<br />
♦ Reactive process (benign)<br />
♦<br />
♦<br />
♦<br />
♦<br />
♦<br />
Sarcoidosis<br />
Hypersensitivity reaction to medications<br />
Serum sickness<br />
Rheumatoid arthritis<br />
Castleman disease<br />
P: Plan<br />
Diagnostic Evaluation<br />
After <strong>the</strong> history and physical examination, <strong>the</strong> cause <strong>of</strong><br />
lymphadenopathy may be clear and fur<strong>the</strong>r diagnostic<br />
testing may not be necessary. If <strong>the</strong> cause <strong>of</strong> <strong>the</strong><br />
lymphadenopathy is still uncertain, per<strong>for</strong>m diagnostic<br />
testing as indicated by <strong>the</strong> patient’s presentation. This<br />
may include <strong>the</strong> following tests:<br />
♦<br />
♦<br />
♦<br />
♦<br />
♦<br />
♦<br />
♦<br />
CD4 count (with or without <strong>HIV</strong> viral load), to<br />
determine <strong>the</strong> risk <strong>of</strong> opportunistic illnesses<br />
Complete blood count with differential; liver<br />
function tests; urinalysis<br />
Chest x-ray<br />
Tuberculin skin test (purified protein derivative, or<br />
PPD)<br />
Rapid plasma reagin (RPR) or Venereal Disease<br />
Research Laboratory (VDRL) test<br />
Blood cultures, if patient is febrile (bacterial,<br />
mycobacterial, and fungal, as indicated)<br />
Testing <strong>for</strong> specific infections if suspected (eg,<br />
Bartonella or LGV)<br />
If a node is large, fixed, nontender, or o<strong>the</strong>rwise<br />
worrisome, or if <strong>the</strong> diagnosis is unclear after initial<br />
evaluation, fine-needle aspiration (FNA) biopsy may<br />
provide a diagnosis. If FNA is nondiagnostic (falsenegative<br />
results are relatively <strong>com</strong>mon), obtain an open<br />
biopsy <strong>for</strong> definitive evaluation. Biopsy specimens<br />
should be sent <strong>for</strong> bacterial, mycobacterial, and fungal<br />
cultures; acid-fast staining <strong>for</strong> mycobacteria; and<br />
cytologic examination.<br />
If a node is large, inflamed, tender, or fluctuant, and<br />
a bacterial infection is suspected, consider initiating<br />
empiric antibiotic treatment and monitoring <strong>the</strong><br />
patient over 1-2 weeks. If <strong>the</strong> node does not respond<br />
to antibiotic treatment or <strong>the</strong> patient be<strong>com</strong>es more<br />
symptomatic, arrange <strong>for</strong> FNA or open biopsy to<br />
establish <strong>the</strong> diagnosis.