Volume 6, Spring 2008 - Saddleback College
Volume 6, Spring 2008 - Saddleback College
Volume 6, Spring 2008 - Saddleback College
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Fall 2007 Biology 3A Abstracts<br />
monitor. A primary blood gas and chemistry was run<br />
on the Nova® (Nova Stat Profile Critical Care Xpress<br />
(CCX), Nova biomedical Corp., Waltham, MA) blood<br />
gas analyzer for basic chemistry and blood gas<br />
analysis. Each sample was spun at an apex of<br />
approximately 6,000 rpm (2,000 x g). Serum was used<br />
to run a full chemistry panel using the Alpha<br />
Washerman® (Alfa Wassermann ACE; Clinical<br />
System, West Caldwell, NJ, USA) blood chemistry<br />
analyzer. These tests were used to establish the overall<br />
internal physiological health of each canine patient.<br />
Only patients found to be within normal ranges met the<br />
criterion for this study. The weight, sex, and breed of<br />
each canine patient was also recorded.<br />
Each experimental subject received a<br />
peripheral intravenous catheter in the left or right<br />
cephalic vein and subsequently placed on Normasol-<br />
R® (Normasol-R; hospera inc., Abbott Laboratories,<br />
Chicago, IL) crystalloid fluid therapy for 1-2 hours preanesthetically<br />
at 2.5 mL/kg/hr.<br />
Patients were anesthetized using a preanesthetic<br />
pain medication, Hydromorphone HCl (2.0-<br />
mg/mL) injectable, administered intravenously (IV),<br />
and dosed by weight at 0.1 mg/kg. Anesthesia was<br />
induced using the IV injectable anesthetic, Propfol<br />
(Proflo®, Abbott Laboratories, North Chicago, IL), at a<br />
dose of 5 mg/kg titrated to effect. Each test subject was<br />
then intubated with a sterile cuffed endotraecheal tube.<br />
Anesthetic was maintained using a gas anesthetic<br />
agent, Isoflurane (IsoFlo®; Abbott Laboratories, North<br />
Chicago, IL USA), which was delivered by a closed<br />
circuit system via a constant flow of oxygen at 2.0<br />
L/min passed through an Isoflurane vaporizer (Drager,<br />
Lubeck, Germany) initially at the rate of 3.0 % ± 1.5 %<br />
(dependent on weight and initial anesthetic depth).<br />
Crystalloid fluid therapy was increased 5 ml/kg/hr<br />
while under anesthesia to ensure proper profusion<br />
during the procedure.<br />
A 25 gauge tuberculin syringe was used to<br />
draw 0.10 mL of blood from the saphenous accessory<br />
vein of the hind limb and added to the lactate testing<br />
strip for lactate analysis. Samples were taken at 20<br />
minute intervals for the remainder of the procedure<br />
including one immediate post-induction sample and<br />
then processed immediately with the Accutrend®<br />
handheld Lactate monitor. Each study patient was<br />
monitored using the LifeWindow 6000V vital signs<br />
monitor (multi-parameter patient monitor, LW6000;<br />
Digicare Biomedical Technology, West Palm Beach,<br />
FL), in addition to visual supervision by the veterinary<br />
surgical nurse and veterinarian. Heart rate (Beats Per<br />
Minute), blood pressure (mmHg), respiratory rate<br />
(Breaths Per Minute), ETCO 2 (%), SPO 2 (%),<br />
temperature (ºF), IV fluid rate (mL/hr), anesthetic level<br />
79<br />
<strong>Saddleback</strong> Journal of Biology<br />
<strong>Spring</strong> <strong>2008</strong><br />
(%), O 2 level, and blood lactate levels were measured<br />
and recorded at specific time intervals throughout the<br />
procedure. Each patient received heat support via a<br />
warm air delivery system and a heated surgical table<br />
(Bair Hugger®; Arizant Healthcare Inc., Eden Prairie,<br />
MN), during the anesthetic procedure.<br />
Results<br />
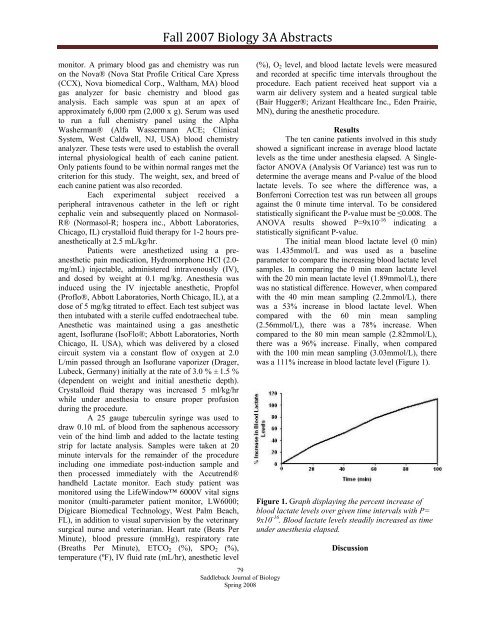
The ten canine patients involved in this study<br />
showed a significant increase in average blood lactate<br />
levels as the time under anesthesia elapsed. A Singlefactor<br />
ANOVA (Analysis Of Variance) test was run to<br />
determine the average means and P-value of the blood<br />
lactate levels. To see where the difference was, a<br />
Bonferroni Correction test was run between all groups<br />
against the 0 minute time interval. To be considered<br />
statistically significant the P-value must be ≤0.008. The<br />
ANOVA results showed P=9x10 -16 indicating a<br />
statistically significant P-value.<br />
The initial mean blood lactate level (0 min)<br />
was 1.435mmol/L and was used as a baseline<br />
parameter to compare the increasing blood lactate level<br />
samples. In comparing the 0 min mean lactate level<br />
with the 20 min mean lactate level (1.89mmol/L), there<br />
was no statistical difference. However, when compared<br />
with the 40 min mean sampling (2.2mmol/L), there<br />
was a 53% increase in blood lactate level. When<br />
compared with the 60 min mean sampling<br />
(2.56mmol/L), there was a 78% increase. When<br />
compared to the 80 min mean sample (2.82mmol/L),<br />
there was a 96% increase. Finally, when compared<br />
with the 100 min mean sampling (3.03mmol/L), there<br />
was a 111% increase in blood lactate level (Figure 1).<br />
Figure 1. Graph displaying the percent increase of<br />
blood lactate levels over given time intervals with P=<br />
9x10 -16 . Blood lactate levels steadily increased as time<br />
under anesthesia elapsed.<br />
Discussion