- Page 1:
Brian P. Jacob · David C. Chen Bru
- Page 5 and 6:
The SAGES Manual of Groin Pain Bria
- Page 7 and 8:
Foreword Inguinal hernia repair is
- Page 9 and 10:
Contents Part I Primary Groin Pain
- Page 11 and 12:
Contents ix 22 Management of Inguin
- Page 13:
Contents xi 45 Value-Based Clinical
- Page 16 and 17:
xiv Editors and Contributors Jeffre
- Page 18 and 19:
xvi Editors and Contributors David
- Page 20 and 21:
xviii Editors and Contributors Greg
- Page 22 and 23:
xx Editors and Contributors David S
- Page 24 and 25:
1. Introduction to Primary and Seco
- Page 26 and 27:
1. Introduction to Primary and Seco
- Page 28 and 29:
1. Introduction to Primary and Seco
- Page 30 and 31:
10 I.A. Gawlas and W.J. Peacock Ili
- Page 32 and 33:
12 I.A. Gawlas and W.J. Peacock Tra
- Page 34 and 35:
14 I.A. Gawlas and W.J. Peacock Var
- Page 36 and 37:
3. Complex Regional Pain Syndrome T
- Page 38 and 39:
3. Complex Regional Pain Syndrome T
- Page 40 and 41:
3. Complex Regional Pain Syndrome T
- Page 42 and 43:
3. Complex Regional Pain Syndrome T
- Page 44 and 45:
3. Complex Regional Pain Syndrome T
- Page 46 and 47:
4. Chief Complaint of Groin Pain: H
- Page 48 and 49:
4. Chief Complaint of Groin Pain…
- Page 50 and 51:
4. Chief Complaint of Groin Pain…
- Page 52 and 53:
4. Chief Complaint of Groin Pain…
- Page 54 and 55:
4. Chief Complaint of Groin Pain…
- Page 56 and 57:
4. Chief Complaint of Groin Pain…
- Page 58 and 59:
4. Chief Complaint of Groin Pain…
- Page 60 and 61:
42 C. Ma and A. Ramaswamy inguinal
- Page 62 and 63:
44 C. Ma and A. Ramaswamy Categoriz
- Page 64 and 65:
46 C. Ma and A. Ramaswamy with no s
- Page 66 and 67:
48 C. Ma and A. Ramaswamy 26. Aasva
- Page 68 and 69:
50 I.M. Daoud and K. Dunn Other per
- Page 70 and 71:
52 I.M. Daoud and K. Dunn low herni
- Page 72 and 73:
54 I.M. Daoud and K. Dunn In the po
- Page 74 and 75:
56 I.M. Daoud and K. Dunn with a he
- Page 76 and 77:
58 I.M. Daoud and K. Dunn 13. O’C
- Page 78 and 79:
60 G.J. Mancini Occult Hernia Backg
- Page 80 and 81:
62 G.J. Mancini Magnetic resonance
- Page 82 and 83:
64 G.J. Mancini rocking motion can
- Page 84 and 85:
66 G.J. Mancini Unique to the adduc
- Page 86 and 87:
68 G.J. Mancini two nerve injuries
- Page 88 and 89:
70 G.J. Mancini abdominis has a rep
- Page 90 and 91:
72 G.J. Mancini 5. Light D, Ratnasi
- Page 92 and 93:
74 J.C. Campbell and G.D. Paiement
- Page 94 and 95:
76 J.C. Campbell and G.D. Paiement
- Page 96 and 97:
78 J.C. Campbell and G.D. Paiement
- Page 98 and 99:
80 J.C. Campbell and G.D. Paiement
- Page 100 and 101:
82 J.C. Campbell and G.D. Paiement
- Page 102 and 103:
84 J.C. Campbell and G.D. Paiement
- Page 104 and 105:
86 J.C. Campbell and G.D. Paiement
- Page 106 and 107:
88 J.C. Campbell and G.D. Paiement
- Page 108 and 109:
90 J.C. Campbell and G.D. Paiement
- Page 110 and 111:
92 J.C. Campbell and G.D. Paiement
- Page 112 and 113:
94 J.C. Campbell and G.D. Paiement
- Page 114 and 115:
96 J.C. Campbell and G.D. Paiement
- Page 116 and 117:
98 J.C. Campbell and G.D. Paiement
- Page 118 and 119:
100 J.C. Campbell and G.D. Paiement
- Page 120 and 121: 9. Groin Pain Etiology: Spine and B
- Page 122 and 123: 9. Groin Pain Etiology: Spine and B
- Page 124 and 125: 9. Groin Pain Etiology: Spine and B
- Page 126 and 127: 9. Groin Pain Etiology: Spine and B
- Page 128 and 129: 10. Groin Pain Etiology: Spermatic
- Page 130 and 131: Table 10.2. European Association of
- Page 132 and 133: 10. Groin Pain Etiology: Spermatic
- Page 134 and 135: 10. Groin Pain Etiology: Spermatic
- Page 136 and 137: 10. Groin Pain Etiology: Spermatic
- Page 138 and 139: 10. Groin Pain Etiology: Spermatic
- Page 140 and 141: 10. Groin Pain Etiology: Spermatic
- Page 142 and 143: 10. Groin Pain Etiology: Spermatic
- Page 144 and 145: 10. Groin Pain Etiology: Spermatic
- Page 146 and 147: 10. Groin Pain Etiology: Spermatic
- Page 148 and 149: 10. Groin Pain Etiology: Spermatic
- Page 150 and 151: 10. Groin Pain Etiology: Spermatic
- Page 152 and 153: 10. Groin Pain Etiology: Spermatic
- Page 154 and 155: 138 M. Hibner and C. Coyne Piriform
- Page 156 and 157: 140 M. Hibner and C. Coyne Fig. 11.
- Page 158 and 159: 142 M. Hibner and C. Coyne Table 11
- Page 160 and 161: 144 M. Hibner and C. Coyne present
- Page 162 and 163: 146 M. Hibner and C. Coyne Table 11
- Page 164 and 165: 148 M. Hibner and C. Coyne Once the
- Page 166 and 167: 150 M. Hibner and C. Coyne 3. Hibne
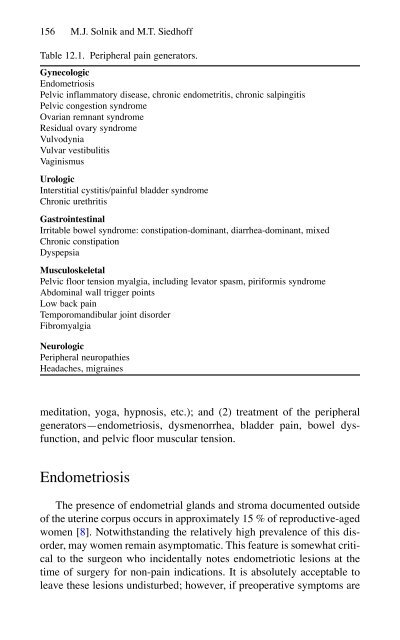
- Page 168 and 169: 12. Chronic Pelvic Pain in Women M.
- Page 172 and 173: 12. Chronic Pelvic Pain in Women 15
- Page 174 and 175: 12. Chronic Pelvic Pain in Women 15
- Page 176 and 177: 12. Chronic Pelvic Pain in Women 16
- Page 178 and 179: 12. Chronic Pelvic Pain in Women 16
- Page 180 and 181: 12. Chronic Pelvic Pain in Women 16
- Page 182 and 183: 12. Chronic Pelvic Pain in Women 16
- Page 184 and 185: 12. Chronic Pelvic Pain in Women 16
- Page 186 and 187: 12. Chronic Pelvic Pain in Women 17
- Page 188 and 189: 174 J.M. Miller et al. Knowing the
- Page 190 and 191: 176 J.M. Miller et al. Fig. 13.2. A
- Page 192 and 193: 178 J.M. Miller et al. Fig. 13.4. A
- Page 194 and 195: 180 J.M. Miller et al. Fig. 13.7. A
- Page 196 and 197: 182 J.M. Miller et al. Fig. 13.9. C
- Page 198 and 199: 184 J.M. Miller et al. Fig. 13.14.
- Page 200 and 201: 186 J.M. Miller et al. Fig. 13.15.
- Page 202 and 203: 188 J.M. Miller et al. Fig. 13.20.
- Page 204 and 205: 190 J.M. Miller et al. Fig. 13.22.
- Page 206 and 207: 192 J.M. Miller et al. Cardiac Cath
- Page 208 and 209: 194 B.J. Dunkin Noxious peripheral
- Page 210 and 211: 196 B.J. Dunkin Table 14.1. Summary
- Page 212 and 213: 198 B.J. Dunkin Rectus abdominis Ex
- Page 214 and 215: 200 B.J. Dunkin COX-1 COX-2 Celecpx
- Page 216 and 217: 202 B.J. Dunkin Table 14.2. Common
- Page 218 and 219: 204 B.J. Dunkin Possible Preoperati
- Page 220 and 221:
206 B.J. Dunkin Postoperative Pain
- Page 222 and 223:
208 B.J. Dunkin Summary Understandi
- Page 224 and 225:
15. Chronic Groin Pain Following An
- Page 226 and 227:
15. Chronic Groin Pain Following An
- Page 228 and 229:
15. Chronic Groin Pain Following An
- Page 230 and 231:
15. Chronic Groin Pain Following An
- Page 232 and 233:
15. Chronic Groin Pain Following An
- Page 234 and 235:
222 E.L. Felix not seem to alter th
- Page 236 and 237:
224 E.L. Felix nerves from the surg
- Page 238 and 239:
226 E.L. Felix Fig. 16.2. Lateral f
- Page 240 and 241:
228 E.L. Felix It has been establis
- Page 242 and 243:
230 E.L. Felix 18. Pollak R, Nyhus
- Page 244 and 245:
17. The Orthopedic Perspective on G
- Page 246 and 247:
17. The Orthopedic Perspective on G
- Page 248 and 249:
17. The Orthopedic Perspective on G
- Page 250 and 251:
17. The Orthopedic Perspective on G
- Page 252 and 253:
17. The Orthopedic Perspective on G
- Page 254 and 255:
17. The Orthopedic Perspective on G
- Page 256 and 257:
246 J.F.M. Lange Jr. examination an
- Page 258 and 259:
248 J.F.M. Lange Jr. and remedial s
- Page 260 and 261:
250 J.F.M. Lange Jr. Best available
- Page 262 and 263:
252 J.F.M. Lange Jr. Neuropathic pa
- Page 264 and 265:
254 J.F.M. Lange Jr. This algorithm
- Page 266 and 267:
19. Radiologic Evaluation for Posto
- Page 268 and 269:
19 Radiologic Evaluation for Postop
- Page 270 and 271:
19 Radiologic Evaluation for Postop
- Page 272 and 273:
19 Radiologic Evaluation for Postop
- Page 274 and 275:
19 Radiologic Evaluation for Postop
- Page 276 and 277:
268 A. Malhotra extended variant of
- Page 278 and 279:
270 A. Malhotra steroid injections,
- Page 280 and 281:
272 A. Malhotra located just below
- Page 282 and 283:
274 A. Malhotra Nociceptive Acute N
- Page 284 and 285:
276 A. Malhotra 20. Rozen D, Parvez
- Page 286 and 287:
278 R. Álvarez intentionally or in
- Page 288 and 289:
Fig. 21.1. Material: A ballpoint pe
- Page 290 and 291:
Fig. 21.5. Dermatome mapping compat
- Page 292 and 293:
Fig. 21.9. Dermatome mapping compat
- Page 294 and 295:
286 R. Álvarez Subsequently, we mu
- Page 296 and 297:
288 R. Álvarez G : Granuloma H : H
- Page 298 and 299:
290 R. Álvarez Fig. 21.14. Same pa
- Page 300 and 301:
292 R. Álvarez 6. Lermite E, Arnau
- Page 302 and 303:
294 K.A. Seymour and J.S. Yoo Table
- Page 304 and 305:
296 K.A. Seymour and J.S. Yoo repro
- Page 306 and 307:
298 K.A. Seymour and J.S. Yoo Recur
- Page 308 and 309:
23. Mesh Removal for Chronic Pain:
- Page 310 and 311:
23. Mesh Removal for Chronic Pain
- Page 312 and 313:
23. Mesh Removal for Chronic Pain
- Page 314 and 315:
23. Mesh Removal for Chronic Pain
- Page 316 and 317:
23. Mesh Removal for Chronic Pain
- Page 318 and 319:
23. Mesh Removal for Chronic Pain
- Page 320 and 321:
23. Mesh Removal for Chronic Pain
- Page 322 and 323:
23. Mesh Removal for Chronic Pain
- Page 324 and 325:
23. Mesh Removal for Chronic Pain
- Page 326 and 327:
320 I.T. MacQueen et al. inguinodyn
- Page 328 and 329:
322 I.T. MacQueen et al. Fig. 24.2.
- Page 330 and 331:
324 I.T. MacQueen et al. Timing and
- Page 332 and 333:
326 I.T. MacQueen et al. Fig. 24.4.
- Page 334 and 335:
328 I.T. MacQueen et al. Posthernio
- Page 336 and 337:
330 I.T. MacQueen et al. never be e
- Page 338 and 339:
25. Laparoscopic Triple Neurectomy
- Page 340 and 341:
25. Laparoscopic Triple Neurectomy
- Page 342 and 343:
25. Laparoscopic Triple Neurectomy
- Page 344 and 345:
25. Laparoscopic Triple Neurectomy
- Page 346 and 347:
25. Laparoscopic Triple Neurectomy
- Page 348 and 349:
26. Chronic Orchialgia: Workup and
- Page 350 and 351:
26. Chronic Orchialgia: Workup and
- Page 352 and 353:
26. Chronic Orchialgia: Workup and
- Page 354 and 355:
26. Chronic Orchialgia: Workup and
- Page 356 and 357:
26. Chronic Orchialgia: Workup and
- Page 358 and 359:
26. Chronic Orchialgia: Workup and
- Page 360 and 361:
26. Chronic Orchialgia: Workup and
- Page 362 and 363:
26. Chronic Orchialgia: Workup and
- Page 364 and 365:
26. Chronic Orchialgia: Workup and
- Page 366 and 367:
26. Chronic Orchialgia: Workup and
- Page 368 and 369:
27. The Role of Bioactive Prostheti
- Page 370 and 371:
27. The Role of Bioactive Prostheti
- Page 372 and 373:
27. The Role of Bioactive Prostheti
- Page 374 and 375:
27. The Role of Bioactive Prostheti
- Page 376 and 377:
27. The Role of Bioactive Prostheti
- Page 378 and 379:
376 G. Campanelli et al. affecting
- Page 380 and 381:
378 G. Campanelli et al. into the w
- Page 382 and 383:
380 G. Campanelli et al. chronic gr
- Page 384 and 385:
382 G. Campanelli et al. A prospect
- Page 386 and 387:
384 G. Campanelli et al. open mesh
- Page 388 and 389:
386 G. Campanelli et al. 38. Alfier
- Page 390 and 391:
29. Prevention of Pain: Optimizing
- Page 392 and 393:
29. Prevention of Pain: Optimizing
- Page 394 and 395:
29. Prevention of Pain: Optimizing
- Page 396 and 397:
29. Prevention of Pain: Optimizing
- Page 398 and 399:
30. Prophylactic Neurectomy Versus
- Page 400 and 401:
30. Prophylactic Neurectomy Versus
- Page 402 and 403:
30. Prophylactic Neurectomy Versus
- Page 404 and 405:
30. Prophylactic Neurectomy Versus
- Page 406 and 407:
Table 31.1. Selective neurectomy wi
- Page 408 and 409:
408 W.M.J. Reinpold and A.D. Schroe
- Page 410 and 411:
410 W.M.J. Reinpold and A.D. Schroe
- Page 412 and 413:
412 W.M.J. Reinpold and A.D. Schroe
- Page 414 and 415:
414 W.M.J. Reinpold and A.D. Schroe
- Page 416 and 417:
32. Chronic Groin Pain: Mesh or No
- Page 418 and 419:
32. Chronic Groin Pain: Mesh or No
- Page 420 and 421:
32. Chronic Groin Pain: Mesh or No
- Page 422 and 423:
32. Chronic Groin Pain: Mesh or No
- Page 424 and 425:
32. Chronic Groin Pain: Mesh or No
- Page 426 and 427:
Part IV Case Reports and Patients
- Page 428 and 429:
430 S. Towfigh were irregular and s
- Page 430 and 431:
432 S. Towfigh in addressing her sy
- Page 432 and 433:
434 S. Towfigh Conclusion We have y
- Page 434 and 435:
436 K.W. Kercher Physical Examinati
- Page 436 and 437:
438 K.W. Kercher Fig. 34.4. Left ad
- Page 438 and 439:
440 K.W. Kercher Fig. 34.5. After d
- Page 440 and 441:
442 K.W. Kercher the posterior wall
- Page 442 and 443:
444 K.W. Kercher Table 34.2. Surgic
- Page 444 and 445:
35. Chronic Post-inguinal Herniorrh
- Page 446 and 447:
35 Chronic Post-inguinal Herniorrha
- Page 448 and 449:
35 Chronic Post-inguinal Herniorrha
- Page 450 and 451:
36. Sports Hernia with Adductor Ten
- Page 452 and 453:
36. Sports Hernia with Adductor Ten
- Page 454 and 455:
36. Sports Hernia with Adductor Ten
- Page 456 and 457:
36. Sports Hernia with Adductor Ten
- Page 458 and 459:
36. Sports Hernia with Adductor Ten
- Page 460 and 461:
464 C.G. DuCoin and G.R. Jacobsen P
- Page 462 and 463:
466 C.G. DuCoin and G.R. Jacobsen O
- Page 464 and 465:
468 J.A. Blatnik and A.S. Prabhu a
- Page 466 and 467:
470 J.A. Blatnik and A.S. Prabhu Fi
- Page 468 and 469:
472 J.A. Blatnik and A.S. Prabhu ma
- Page 470 and 471:
474 S. Towfigh Physical Exam The pa
- Page 472 and 473:
476 S. Towfigh The patient’s loca
- Page 474 and 475:
478 S. Towfigh Fig. 39.2. Diagram o
- Page 476 and 477:
480 S. Towfigh periphery. He is 2+
- Page 478 and 479:
482 S. Towfigh References 1. Matthi
- Page 480 and 481:
484 N.A. Al-Enazi and B.P. Jacob
- Page 482 and 483:
486 N.A. Al-Enazi and B.P. Jacob Fi
- Page 484 and 485:
488 N.A. Al-Enazi and B.P. Jacob pu
- Page 486 and 487:
42. Patient with Chronic Pelvic Pai
- Page 488 and 489:
42. Patient with Chronic Pelvic Pai
- Page 490 and 491:
43. Thoracolumbar Syndrome James A.
- Page 492 and 493:
43. Thoracolumbar Syndrome 497 The
- Page 494 and 495:
43. Thoracolumbar Syndrome 499 Groi
- Page 496 and 497:
44. Patient with Referred Hip Pain
- Page 498 and 499:
44. Patient with Referred Hip Pain
- Page 500 and 501:
45. Value-Based Clinical Quality Im
- Page 502 and 503:
45. Value-Based Clinical Quality Im
- Page 504 and 505:
45. Value-Based Clinical Quality Im
- Page 506 and 507:
45. Value-Based Clinical Quality Im
- Page 508 and 509:
45. Value-Based Clinical Quality Im
- Page 510 and 511:
46. Patient Care Manager Perspectiv
- Page 512 and 513:
46. Patient Care Manager Perspectiv
- Page 514 and 515:
46. Patient Care Manager Perspectiv
- Page 516 and 517:
46. Patient Care Manager Perspectiv
- Page 518 and 519:
47. Workers’ Compensation: An Occ
- Page 520 and 521:
47. Workers’ Compensation: An Occ
- Page 522 and 523:
47. Workers’ Compensation: An Occ
- Page 524 and 525:
47. Workers’ Compensation: An Occ
- Page 526 and 527:
532 Index Athletic pubalgia (cont.)
- Page 528 and 529:
534 Index Chronic post-herniorrhaph
- Page 530 and 531:
536 Index Groin pain (cont.) magnet
- Page 532 and 533:
538 Index Ilioinguinal nerve (IIN)
- Page 534 and 535:
540 Index Local anesthetics (cont.)
- Page 536 and 537:
542 Index Peripheral nerve entrapme
- Page 538 and 539:
544 Index S Sacroiliac (SI) joint d
- Page 540:
546 Index Transperineal pudendal ne