12th Congress of the European Hematology ... - Haematologica
12th Congress of the European Hematology ... - Haematologica
12th Congress of the European Hematology ... - Haematologica
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
12 th <strong>Congress</strong> <strong>of</strong> <strong>the</strong> <strong>European</strong> <strong>Hematology</strong> Association<br />
11% and lipase elevations in 15% <strong>of</strong> nilotinib pts (1 patient developed<br />
Grade 1/2 pancreatitis; no Grade 3/4 pancreatitis), while dasatinib abnormalities<br />
are hypophosphatemia in 11% and hypocalcemia in 22%. Rates<br />
<strong>of</strong> Grade 3/4 non-hematologic AEs such as pleural effusion, GI bleeding,<br />
arrhythmia, and pneumonia/infection are >2-7 times higher for dasatinib<br />
than nilotinib. Summary and Conclusions. The toxicity pr<strong>of</strong>iles <strong>of</strong> <strong>the</strong> second<br />
generation TKIs for imatinib resistant/intolerant CML-CP appear to<br />
be different and favor nilotinib with its reduced rates <strong>of</strong> Grade 3/4 AEs<br />
even with longer median duration <strong>of</strong> drug exposure compared to dasatinib.<br />
Fur<strong>the</strong>r analysis is required to understand <strong>the</strong> cost impact to health<br />
care payers <strong>of</strong> <strong>the</strong> differences in safety pr<strong>of</strong>iles among <strong>the</strong> new TKIs.<br />
Table 1.<br />
0553<br />
WITHIN THE P-LOOP GROUP, THE Y253H AND E255K/V ABL KINASE DOMAIN<br />
MUTATIONS ARE OF PARTICULAR SEVERE PROGNOSIS IN CHRONIC MYELOGENOUS<br />
LEUKEMIA PATIENTS RESISTANT TO IMATINIB MESYLATE<br />
F. Nicolini, 1 F.E. Nicolini, 1 S. Corm, 2 S. Hayette, 3 Q.H. Le,1 D. Bories, 4<br />
S. Giraudier, 4 M. Tulliez, 4 N. Sorel, 5 F. Guilhot, 5 D. Rea, 6<br />
J-M. Cayuela, 6 P. Rousselot, 7 M.P. Gaub, 8 F. Maloisel, 8 F.X. Mahon, 9<br />
L. Legros, 10 P. Cony-Makhoul, 11 J.J. Kiladjian, 12 O. Tournilhac, 13<br />
D. Guyotat, 14 M. Delain, 15 V. Leblond, 16 B. Varet, 17 M. Michallet, 1<br />
C. Roche-Lestienne, 18 C. Preudhomme18 1 Edouard Herriot Hospital, LYON; 2 Hôpital Huriez, LILLE; 3 Centre Hospitalier<br />
Lyon Sud, PIERRE-BENITE; 4 Hôpital Henri Mondor, CRETEIL; 5 Hôpital<br />
Jean Bernard, POITIERS; 6 Hôpital Saint Louis, PARIS; 7 Hospital Jean Mignot,<br />
LE CHESNAY; 8 Hôpital Civil, STRASBOURG; 9 Hôpital Pellegrin, BOR-<br />
DEAUX; 10 Hôpital de l'Archet, NICE; 11 Centre Hospitalier, ANNECY; 12 Hôpital<br />
Avicenne, BOBIGNY; 13 Hôtal Dieu, CLERMONT-FERRAND; 14 ICL,<br />
SAINT-ETIENNE; 15 Hôpital Bretonneau, TOURS; 16 Pitié Salpêtrière Hospital,<br />
PARIS; 17 Hôpital Necker, PARIS; 18 Hôpital Calmette, LILLE, France,<br />
Despite its remarkable efficacy in chronic myelogenous leukemia<br />
(CML) resistance to imatinib mesylate (IM) may arise, and <strong>the</strong> onset <strong>of</strong><br />
BCR-ABL point mutations remains <strong>the</strong> main cause identified, being<br />
responsible for resistance. Among <strong>the</strong>se mutations, some located in <strong>the</strong><br />
ATP binding loop (P-loop: residues 248-255) or at residue 315 seem particularly<br />
critical by disturbing IM binding or by altering <strong>the</strong> flexibility <strong>of</strong><br />
<strong>the</strong> ABL kinase domain. The poor clinical prognosis <strong>of</strong> <strong>the</strong>se mutations<br />
is generally accepted but still debatable. Among <strong>the</strong> P-loop group, biochemistry<br />
and cellular assays suggest that <strong>the</strong>re is some heterogeneity<br />
in impairing <strong>the</strong> response to IM and mutations located at residues 253<br />
and 255 are responsible for particularly high IC50 values in vitro. In a vast<br />
retrospective study from 5 different French centers, we analysed and<br />
compared <strong>the</strong> features and clinical outcomes <strong>of</strong> 75 CML patients treated<br />
with IM and presenting ei<strong>the</strong>r clinical, cytological, cytogenetical<br />
resistance or molecular progression. Progression has been defined as a<br />
loss <strong>of</strong> any previous response, progression to a more advanced phase and<br />
a ≥2-fold increase in BCR-ABL/ABL ratio confirmed on 2 assessments 3<br />
months apart. Fourty-six patients (32M/14F, median age 52) harboured<br />
49 P-loop mutations [Group 1 (G1)] and 29 patients (19M/10F, median<br />
age 52) harboured 37 mutations with at least a T315I mutation (± o<strong>the</strong>r)<br />
[Group 2 (G2)], as detected by direct sequencing. At mutation discov-<br />
206 | haematologica/<strong>the</strong> hematology journal | 2007; 92(s1)<br />
ery 24 patients (52%) were in chronic phase (CP), 12 (26%) in accelerated<br />
phase (AP), 10 (22%) in blast crisis (BC) in G1 and 12 (41%), 4<br />
(14%), 13 (45%) in G2 respectively. The median duration <strong>of</strong> IM was 16<br />
months (1.3-65.6) for G1 and 19 (0-57.6) for G2 (p=ns). In patients who<br />
had received IFN prior to IM, duration <strong>of</strong> IFN was similar between <strong>the</strong><br />
2 groups (5 months (0-89) for G1 vs 9 months (0-131) for G2, p=ns). The<br />
median interval between diagnosis and day 1 <strong>of</strong> IM was 16 months (0-<br />
61.5) for G1 and 13 months (0-49.5) (p=ns) for G2. Univariate analysis<br />
for gender, age, sokal, prior treatment with IFN, initial dose <strong>of</strong> IM, intervals<br />
between diagnosis-IM start, diagnosis-mutation detection, IMmutation<br />
detection and major cytogenetic response with IM, did not<br />
show any significant impact <strong>of</strong> <strong>the</strong>se variables. Multivariate analysis<br />
demonstrated a significantly worse PFS since IM start for E255K/<br />
V+Y253H mutants vs o<strong>the</strong>r P-loop mutants (p=0.016, HR:2.96, 95%CI:<br />
1.22-7.16). IFN treatment prior to IM was associated with better survival<br />
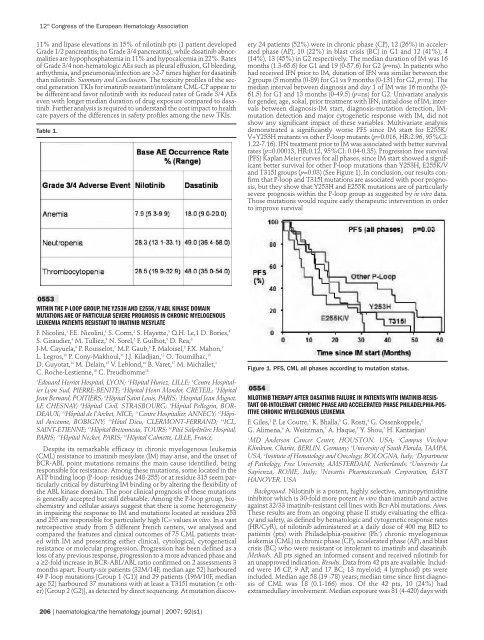
rates (p=0.00013, HR:0.12, 95%CI: 0.04-0.35). Progression free survival<br />
(PFS) Kaplan Meier curves for all phases, since IM start showed a significant<br />
better survival for o<strong>the</strong>r P-loop mutations than Y253H, E255K/V<br />
and T315I groups (p=0.03) (See Figure 1). In conclusion, our results confirm<br />
that P-loop and T315I mutations are associated with poor prognosis,<br />
but <strong>the</strong>y show that Y253H and E255K mutations are <strong>of</strong> particularly<br />
severe prognosis within <strong>the</strong> P-loop group as suggested by in vitro data.<br />
Those mutations would require early <strong>the</strong>rapeutic intervention in order<br />
to improve survival<br />
Figure 1. PFS, CML all phases according to mutation status.<br />
0554<br />
NILOTINIB THERAPY AFTER DASATINIB FAILURE IN PATIENTS WITH IMATINIB-RESIS-<br />
TANT OR-INTOLERANT CHRONIC PHASE AND ACCELERATED PHASE PHILADELPHIA-POS-<br />
ITIVE CHRONIC MYELOGENOUS LEUKEMIA<br />
F. Giles, 1 P. Le Coutre, 2 K. Bhalla, 3 G. Rosti, 4 G. Ossenkoppele, 5<br />
G. Alimena, 6 A. Weitzman, 7 A. Haque, 7 Y. Shou, 7 H. Kantarjian1 1 MD Anderson Cancer Center, HOUSTON, USA; 2 Campus Virchow<br />
Klinikum, Charite, BERLIN, Germany; 3 University <strong>of</strong> South Florida, TAMPA,<br />
USA, 4 Institute <strong>of</strong> <strong>Hematology</strong> and Oncology, BOLOGNA, Italy; 5 Department<br />
<strong>of</strong> Pathology, Free University, AMSTERDAM, Ne<strong>the</strong>rlands; 6 University La<br />
Sapienza, ROME, Italy; 7 Novartis Pharmaceuticals Corporation, EAST<br />
HANOVER, USA<br />
Background. Nilotinib is a potent, highly selective, aminopyrimidine<br />
inhibitor which is 30-fold more potent in vitro than imatinib and active<br />
against 32/33 imatinib-resistant cell lines with Bcr-Abl mutations. Aims.<br />
These results are from an ongoing phase II study evaluating <strong>the</strong> efficacy<br />
and safety, as defined by hematologic and cytogenetic response rates<br />
(HR/CyR), <strong>of</strong> nilotinib administered at a daily dose <strong>of</strong> 400 mg BID to<br />
patients (pts) with Philadelphia-positive (Ph + ) chronic myelogenous<br />
leukemia (CML) in chronic phase (CP), accelerated phase (AP), and blast<br />
crisis (BC) who were resistant or intolerant to imatinib and dasatinib.<br />
Methods. All pts signed an informed consent and received nilotinib for<br />
an unapproved indication. Results. Data from 42 pts are available. Included<br />
were 16 CP, 9 AP, and 17 BC; 13 myeloid; 4 lymphoid) pts were<br />
included. Median age 58 (19 -78) years; median time since first diagnosis<br />
<strong>of</strong> CML was 18 (0.1-166) mos. Of <strong>the</strong> 42 pts, 10 (24%) had<br />
extramedullary involvement. Median exposure was 81 (4-420) days with