12th Congress of the European Hematology ... - Haematologica
12th Congress of the European Hematology ... - Haematologica
12th Congress of the European Hematology ... - Haematologica
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
12 th <strong>Congress</strong> <strong>of</strong> <strong>the</strong> <strong>European</strong> <strong>Hematology</strong> Association<br />
men. Phase 1 (immuno-chemo<strong>the</strong>rapy), consisted <strong>of</strong> 2-4 courses with<br />
Rituximab day 1, vincristine day 2, and cyclophosphamide day 2 to 6.<br />
Phase 2 (in vivo purging and PBSC mobilization), coupled Rituximab on<br />
days 1 and 9 with HD-AraC (2 g/m 2 every 12 h on days 2 and 3). Phase<br />
3 (high-dose chemo<strong>the</strong>rapy with autotransplant) consisted <strong>of</strong> BEAM<br />
followed by infusion <strong>of</strong> in vivo purged PBSC plus 2 consolidation doses<br />
<strong>of</strong> Rituximab on days +14 and +21 posttransplant. Results. Median age<br />
50. Histology: 29 grade I, 27 grade II, 8 grade III; 84% stage III-IV; 56%<br />
had bone marrow involvement; 59% were PCR + for bcl-2 rearrangement<br />
in blood and/or marrow. At enrollment, FLIPI was low in 44%,<br />
intermediate in 34%, high in 11%, NA in 11%. Of 64 patients, after<br />
debulking 7 reached CR, 52 PR, and 5 stable disease; <strong>of</strong> 38 PCR+<br />
patients, 9 (24%) achieved molecular response. After immunochemo<strong>the</strong>rapy,<br />
40 patients obtained CR, 22 PR, and 2 progressed; <strong>of</strong> <strong>the</strong><br />
38 PCR + patients, additional 24 achieved molecular response. Overall, 33<br />
patients (87%) were molecularly negative before mobilization. Sixty-one<br />
patients proceeded to PBSC mobilization with in vivo purging. Toxicity<br />
consisted <strong>of</strong> WHO grade 3-4 granulocytopenia in 72%. One patient<br />
who developed E. Coli sepsis during cytopenia did not harvest. Leukaphereses<br />
were started after a median <strong>of</strong> 12 days (range 5-16) after <strong>the</strong> first<br />
dose <strong>of</strong> AraC. The median number <strong>of</strong> CD34 + cells collected was<br />
16.6×10 6 /kg (range 3.8'80.6). All <strong>the</strong> 31 harvests tested for Bcl-2 were<br />
PCR-negative. Autotransplant was performed in 58 patients. The median<br />
time to neutrophils recovery over 0.5×10 9 /L was 10 days (8-14), and<br />
to platelets over 20×10 9 /L was 10 days (6-13). One patient developed<br />
transient cerebral vasculitis during <strong>the</strong> cytopenic phase. The two Rituximab<br />
doses post-transplant did not affect hemopoietic recovery. Asymptomatic<br />
WHO grade 3-4 neutropenia developed in 10 patients after a<br />
median <strong>of</strong> 90 days after transplant. After a median F-U <strong>of</strong> 3.4 years<br />
(range 1-8), 42 patients are in clinical remission (24 for more than 4<br />
years). One patient became PCR + 34 months after transplant without<br />
clinical relapse and was treated with 4 doses <strong>of</strong> Rituximab achieving<br />
PCR – , seven had clinical and molecular recurrence after a median <strong>of</strong> 16<br />
months after transplant (range 5-40). The 5-year event-free survival <strong>of</strong><br />
<strong>the</strong> whole series is 67%. Conclusions. This study demonstrates <strong>the</strong> role<br />
<strong>of</strong> harvesting lymphoma-free PBSC for <strong>the</strong> attainment <strong>of</strong> long-lasting<br />
clinical and molecular responses in refractory/relapsed follicular lymphoma<br />
patients. Asymptomatic late onset neutropenia may occur after<br />
Rituximab consolidation <strong>of</strong> autologous transplant with no clinical influence<br />
on <strong>the</strong> outcome <strong>of</strong> <strong>the</strong> disease.<br />
0730<br />
HEPATITIS C VIRUS INFECTION AND LYMPHOPROLIFERATIVE DISORDERS: A BAYESIAN<br />
APPROACH<br />
L. Arcaini, 1 C. Pascutto, 2 R. Bruno, 3 M. Merli, 2 S. Rizzi, 2 F. Passamonti, 2<br />
E. Rumi, 2 F. Montanari, 2 M. Lucioni, 4 M. Paulli, 4 M. Lazzarino2 1 IRCCS Policlinico S. Matteo Pavia, PAVIA; 2 <strong>Hematology</strong>, IRCCS Policlinico<br />
S. Matteo, PAVIA; 3 Hepatology, IRCCS Policlinico S. Matteo, PAVIA; 4 Pathology,<br />
IRCCS Policlinico S. Matteo, PAVIA, Italy<br />
Background. A recent meta-analysis <strong>of</strong> epidemiologic studies (Dal<br />
Maso 2006) confirmed association between hepatitis C virus (HCV)<br />
infection and lymphoid malignancies but did not identified specific<br />
HCV-related diseases. The Bayesian approach <strong>of</strong>fers an appealing alternative<br />
to classical statistical inference in order to detect specific HCVrelated<br />
type <strong>of</strong> lymphoid neoplasms. Methods. We analysed 2,621<br />
patients with lymphoproliferative disorders diagnosed since 1992 to<br />
2006; HCV serology was available for 1,434 patients. We compared <strong>the</strong><br />
estimates <strong>of</strong> HCV prevalence in each type <strong>of</strong> disorder obtained with<br />
four different statistical models. Model A: <strong>the</strong> classical maximum likelihood<br />
(ML) estimator for <strong>the</strong> binomial distribution, with <strong>the</strong> corresponding<br />
95% confidence intervals. Model B: a fully Bayesian fixed-effects<br />
model based on <strong>the</strong> assumption that <strong>the</strong> number <strong>of</strong> HCV+ patients are<br />
independent binary response variables with group-specific prevalence as<br />
failure probabilities. On each failure probability a non informative prior<br />
distribution was specified. Model C: a fully Bayesian hierarchical<br />
model, based on <strong>the</strong> assumption that all <strong>the</strong> (logistic transformed) prevalence<br />
rates are all drawn from <strong>the</strong> same normally distributed random<br />
variable. The mean <strong>of</strong> <strong>the</strong> random variable is an overall prevalence to be<br />
estimated (with a flat normal hyperprior distribution), and <strong>the</strong> standard<br />
deviation is a random parameter on which a non informative (uniform)<br />
hyperprior distribution has been specified. Model D: a fully Bayesian<br />
hierarchical model, in which <strong>the</strong> (logistic transformed) prevalence <strong>of</strong><br />
each diagnosis group has been assigned to one <strong>of</strong> two normal distributions<br />
with different mean and standard deviation parameters, but with<br />
<strong>the</strong> same non informative hyperpriors as for model C. All Bayesian computations<br />
were carried out using WinBUGS 1.4.1 © Imperial College<br />
272 | haematologica/<strong>the</strong> hematology journal | 2007; 92(s1)<br />
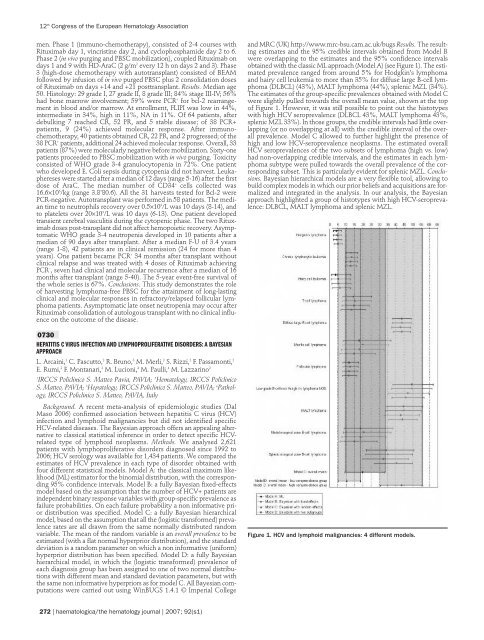
and MRC (UK) http://www.mrc-bsu.cam.ac.uk/bugs Results. The resulting<br />
estimates and <strong>the</strong> 95% credible intervals obtained from Model B<br />
were overlapping to <strong>the</strong> estimates and <strong>the</strong> 95% confidence intervals<br />
obtained with <strong>the</strong> classic ML approach (Model A) (see Figure 1). The estimated<br />
prevalence ranged from around 5% for Hodgkin’s lymphoma<br />
and hairy cell leukemia to more than 35% for diffuse large B-cell lymphoma<br />
(DLBCL) (43%), MALT lymphoma (44%), splenic MZL (34%).<br />
The estimates <strong>of</strong> <strong>the</strong> group-specific prevalences obtained with Model C<br />
were slightly pulled towards <strong>the</strong> overall mean value, shown at <strong>the</strong> top<br />
<strong>of</strong> Figure 1. However, it was still possible to point out <strong>the</strong> histotypes<br />
with high HCV seroprevalence (DLBCL 43%, MALT lymphoma 43%,<br />
splenic MZL 33%). In those groups, <strong>the</strong> credible intervals had little overlapping<br />
(or no overlapping at all) with <strong>the</strong> credible interval <strong>of</strong> <strong>the</strong> overall<br />
prevalence. Model C allowed to fur<strong>the</strong>r highlight <strong>the</strong> presence <strong>of</strong><br />
high and low HCV-seroprevalence neoplasms. The estimated overall<br />
HCV seroprevalences <strong>of</strong> <strong>the</strong> two subsets <strong>of</strong> lymphoma (high vs. low)<br />
had non-overlapping credible intervals, and <strong>the</strong> estimates in each lymphoma<br />
subtype were pulled towards <strong>the</strong> overall prevalence <strong>of</strong> <strong>the</strong> corresponding<br />
subset. This is particularly evident for splenic MZL. Conclusions.<br />
Bayesian hierarchical models are a very flexible tool, allowing to<br />
build complex models in which our prior beliefs and acquisitions are formalized<br />
and integrated in <strong>the</strong> analysis. In our analysis, <strong>the</strong> Bayesian<br />
approach highlighted a group <strong>of</strong> histotypes with high HCV-seroprevalence:<br />
DLBCL, MALT lymphoma and splenic MZL.<br />
Figure 1. HCV and lymphoid malignancies: 4 different models.