Social Insurance and Public Assistance
public-assistance-welfare-reform-colonial-times-to-the-present-ziliak ...
public-assistance-welfare-reform-colonial-times-to-the-present-ziliak ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
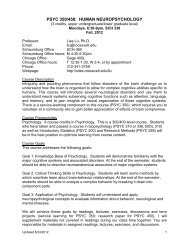
790 Series Bf535–544 Bf SOCIAL INSURANCE AND PUBLIC ASSISTANCE<br />
TABLE Bf535–544 Medicare cost sharing <strong>and</strong> premium amounts: 1966–1999 Continued<br />
Individuals who are eligible for <strong>Social</strong> Security or Railroad Retirement<br />
benefits are eligible for premium-free HI when they reach age 65. Workers<br />
<strong>and</strong> their spouses with a sufficient period of Medicare-only coverage in federal,<br />
state, or local government employment are also eligible at age 65. HI<br />
is also provided to disabled beneficiaries who have been entitled to <strong>Social</strong><br />
Security or Railroad Retirement disability benefits for at least twenty-four<br />
months, <strong>and</strong> government employees with Medicare-only coverage who have<br />
been disabled for more than twenty-nine months. Insured workers <strong>and</strong> their<br />
spouses <strong>and</strong> children who have end-stage renal disease <strong>and</strong> who require kidney<br />
dialysis or a kidney transplant are eligible regardless of age.<br />
Since July 1973, most persons age 65 or older <strong>and</strong> otherwise ineligible<br />
for HIhave been permitted to enroll voluntarily <strong>and</strong> pay the monthly premium<br />
for HI if they also enroll in SMI. Beginning in 1993, Omnibus Budget<br />
Reconciliation legislation stipulated that individuals <strong>and</strong> their spouses with<br />
at least thirty quarters of <strong>Social</strong> Security coverage were eligible for a reduced<br />
premium over the period 1994–1997. The reduced premiums for each year<br />
in this period were $184, $183, $188, <strong>and</strong> $187, respectively.<br />
Financing for the HI program is provided through a tax on earnings that<br />
is separate from the tax used to finance Old-Age, Survivors, <strong>and</strong> Disability<br />
<strong>Insurance</strong> (OASDI) benefits. Prior to January 1991, the OASDI <strong>and</strong> HI<br />
taxes were applied to the same maximum earnings base. Since that time, the<br />
earnings base for HI has increased; the Omnibus Budget Reconciliation Act<br />
of 1993 repealed the dollar limit <strong>and</strong> wages <strong>and</strong> self-employment income<br />
subject to HI taxes. The HI contribution rate of 1.45 percent applies equally<br />
to employers <strong>and</strong> employees, <strong>and</strong> the rate for the self-employed equals the<br />
combined rate of 2.9 percent. Income from contributions is channeled into<br />
the federal HI trust fund, from which HI benefits <strong>and</strong> administrative costs<br />
are paid. After 1977, the Health Care Financing Administration (HCFA) assumed<br />
responsibility for administering the program from the <strong>Social</strong> Security<br />
Administration.<br />
The SMI program covers medically necessary services <strong>and</strong> supplies such<br />
as the following: (1) physician’s, surgeon’s, <strong>and</strong> some Medicare-approved<br />
practitioners’ services; (2) services in an emergency room or outpatient clinic;<br />
(3) laboratory tests, X-rays, <strong>and</strong> other radiology services; (4) mental health<br />
care in a partial hospitalization psychiatric program; (5) ambulatory surgical<br />
center services; (6) physical <strong>and</strong> occupational therapy, <strong>and</strong> speech pathology<br />
services; (7) comprehensive outpatient rehabilitation facility services,<br />
<strong>and</strong> certain treatments of a mental illness; (8) radiation therapy, renal (kidney)<br />
dialysis <strong>and</strong> transplants, <strong>and</strong> heart <strong>and</strong> liver transplant under certain<br />
limited conditions; (9) approved durable medical equipment for home use;<br />
<strong>and</strong> (10) certain drugs <strong>and</strong> biologicals.<br />
Cost-sharing contributions are required for participants in SMI. Beneficiaries<br />
must pay the following: an annual deductible, series Bf540; coinsurance<br />
payments as a percentage of the bill, series Bf541; charges above the<br />
Medicare allowed charge; <strong>and</strong> charges for services that are not covered by<br />
Medicare. Noncovered services include routine physical examinations, longterm<br />
nursing care, <strong>and</strong> certain other health care needs such as eyeglasses. In<br />
addition, the insured pays a monthly premium, series Bf542. The government<br />
then pays a supplemental premium for the aged <strong>and</strong>, since July 1973, for the<br />
disabled, series Bf543–544.<br />
Except for aliens, all persons age 65 <strong>and</strong> older <strong>and</strong> all disabled persons<br />
entitled to coverage under HI are eligible to enroll in the SMI program on a<br />
voluntary basis by paying a monthly premium. Premiums are channeled into<br />
the federal SMI trust fund, <strong>and</strong> the program is administered by HCFA.<br />
Series Bf540–541. Beginning in April 1968, professional inpatient services<br />
of pathologists <strong>and</strong> radiologists were not subject to either a deductible or<br />
coinsurance for SMI. However, after 1980, the pathologists’ <strong>and</strong> radiologists’<br />
services were not subject to a deductible or coinsurance only as long as the<br />
physician accepted assignment (agreed to accept Medicare’s determination<br />
of “reasonable charges” as the full fee for the service). Effective in October<br />
1982, these services once again became subject to coinsurance. In 1973 only,<br />
home health services were not subject to coinsurance under SMI. In 1981<br />
only, home health services were not subject to a deductible.<br />
Series Bf542. In 1973, the monthly premium for SMI for the enrollee was<br />
reduced temporarily to $5.80 in July <strong>and</strong> $6.10 in August by the Cost of Living<br />
Council. For 1989, the monthly premium reported in the table includes<br />
the st<strong>and</strong>ard monthly SMI premium <strong>and</strong> a supplemental monthly flat premium<br />
under the Medicare Catastrophic Coverage Act of 1988. The amount<br />
shown is for most Part B enrollees. Residents of Puerto Rico <strong>and</strong> other territories<br />
<strong>and</strong> commonwealths, as well as other persons enrolled in Part B only,<br />
paid different supplemental flat premiums, so that the amount shown in<br />
the table is larger than the amount paid by these individuals. The Omnibus<br />
Budget Reconciliation Act of 1989 revised the methodology for determining<br />
the 1990 SMI premium for enrollees. Before the revision, the rate would have<br />
been $29.<br />
Series Bf542–543. The monthly premium for SMI for both the enrollee <strong>and</strong><br />
the government did not change to $4 until April 1968.