The report is available in English with a French summary - KCE
The report is available in English with a French summary - KCE
The report is available in English with a French summary - KCE
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>KCE</strong> <strong>report</strong>s 57 Musculoskeletal & Neurological Rehabilitation 57<br />
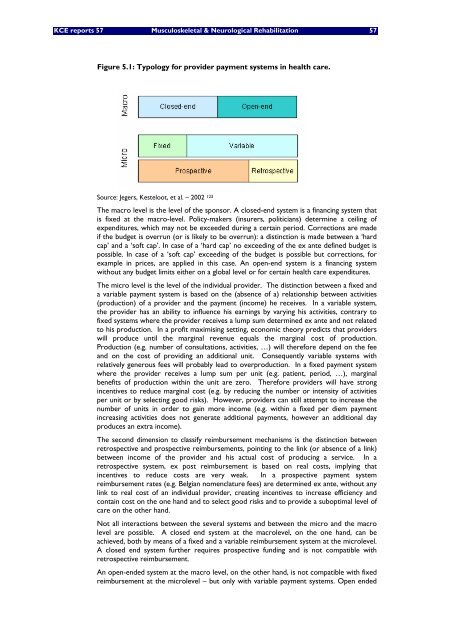
Figure 5.1: Typology for provider payment systems <strong>in</strong> health care.<br />
Source: Jegers, Kesteloot, et al. – 2002 123<br />
<strong>The</strong> macro level <strong>is</strong> the level of the sponsor. A closed-end system <strong>is</strong> a f<strong>in</strong>anc<strong>in</strong>g system that<br />
<strong>is</strong> fixed at the macro-level. Policy-makers (<strong>in</strong>surers, politicians) determ<strong>in</strong>e a ceil<strong>in</strong>g of<br />
expenditures, which may not be exceeded dur<strong>in</strong>g a certa<strong>in</strong> period. Corrections are made<br />
if the budget <strong>is</strong> overrun (or <strong>is</strong> likely to be overrun): a d<strong>is</strong>t<strong>in</strong>ction <strong>is</strong> made between a ‘hard<br />
cap’ and a ‘soft cap’. In case of a ‘hard cap’ no exceed<strong>in</strong>g of the ex ante def<strong>in</strong>ed budget <strong>is</strong><br />
possible. In case of a ‘soft cap’ exceed<strong>in</strong>g of the budget <strong>is</strong> possible but corrections, for<br />
example <strong>in</strong> prices, are applied <strong>in</strong> th<strong>is</strong> case. An open-end system <strong>is</strong> a f<strong>in</strong>anc<strong>in</strong>g system<br />
<strong>with</strong>out any budget limits either on a global level or for certa<strong>in</strong> health care expenditures.<br />
<strong>The</strong> micro level <strong>is</strong> the level of the <strong>in</strong>dividual provider. <strong>The</strong> d<strong>is</strong>t<strong>in</strong>ction between a fixed and<br />
a variable payment system <strong>is</strong> based on the (absence of a) relationship between activities<br />
(production) of a provider and the payment (<strong>in</strong>come) he receives. In a variable system,<br />
the provider has an ability to <strong>in</strong>fluence h<strong>is</strong> earn<strong>in</strong>gs by vary<strong>in</strong>g h<strong>is</strong> activities, contrary to<br />
fixed systems where the provider receives a lump sum determ<strong>in</strong>ed ex ante and not related<br />
to h<strong>is</strong> production. In a profit maxim<strong>is</strong><strong>in</strong>g sett<strong>in</strong>g, economic theory predicts that providers<br />
will produce until the marg<strong>in</strong>al revenue equals the marg<strong>in</strong>al cost of production.<br />
Production (e.g. number of consultations, activities, …) will therefore depend on the fee<br />
and on the cost of provid<strong>in</strong>g an additional unit. Consequently variable systems <strong>with</strong><br />
relatively generous fees will probably lead to overproduction. In a fixed payment system<br />
where the provider receives a lump sum per unit (e.g. patient, period, …), marg<strong>in</strong>al<br />
benefits of production <strong>with</strong><strong>in</strong> the unit are zero. <strong>The</strong>refore providers will have strong<br />
<strong>in</strong>centives to reduce marg<strong>in</strong>al cost (e.g. by reduc<strong>in</strong>g the number or <strong>in</strong>tensity of activities<br />
per unit or by select<strong>in</strong>g good r<strong>is</strong>ks). However, providers can still attempt to <strong>in</strong>crease the<br />
number of units <strong>in</strong> order to ga<strong>in</strong> more <strong>in</strong>come (e.g. <strong>with</strong><strong>in</strong> a fixed per diem payment<br />
<strong>in</strong>creas<strong>in</strong>g activities does not generate additional payments, however an additional day<br />
produces an extra <strong>in</strong>come).<br />
<strong>The</strong> second dimension to classify reimbursement mechan<strong>is</strong>ms <strong>is</strong> the d<strong>is</strong>t<strong>in</strong>ction between<br />
retrospective and prospective reimbursements, po<strong>in</strong>t<strong>in</strong>g to the l<strong>in</strong>k (or absence of a l<strong>in</strong>k)<br />
between <strong>in</strong>come of the provider and h<strong>is</strong> actual cost of produc<strong>in</strong>g a service. In a<br />
retrospective system, ex post reimbursement <strong>is</strong> based on real costs, imply<strong>in</strong>g that<br />
<strong>in</strong>centives to reduce costs are very weak. In a prospective payment system<br />
reimbursement rates (e.g. Belgian nomenclature fees) are determ<strong>in</strong>ed ex ante, <strong>with</strong>out any<br />
l<strong>in</strong>k to real cost of an <strong>in</strong>dividual provider, creat<strong>in</strong>g <strong>in</strong>centives to <strong>in</strong>crease efficiency and<br />
conta<strong>in</strong> cost on the one hand and to select good r<strong>is</strong>ks and to provide a suboptimal level of<br />
care on the other hand.<br />
Not all <strong>in</strong>teractions between the several systems and between the micro and the macro<br />
level are possible. A closed end system at the macrolevel, on the one hand, can be<br />
achieved, both by means of a fixed and a variable reimbursement system at the microlevel.<br />
A closed end system further requires prospective fund<strong>in</strong>g and <strong>is</strong> not compatible <strong>with</strong><br />
retrospective reimbursement.<br />
An open-ended system at the macro level, on the other hand, <strong>is</strong> not compatible <strong>with</strong> fixed<br />
reimbursement at the microlevel – but only <strong>with</strong> variable payment systems. Open ended