- Page 1 and 2:
Systematic review What are the effe
- Page 3 and 4:
Contents List of abbreviations ....
- Page 5 and 6:
List of abbreviations AIDS Acquired
- Page 7 and 8:
Executive summary Background Execut
- Page 9 and 10:
Executive summary be to retrospecti
- Page 11 and 12:
Background many LICs and LMCs, it i
- Page 13 and 14:
Background Cross-sectional surveys
- Page 15 and 16:
Background For some causes of mater
- Page 17 and 18:
Background informal settlements on
- Page 19 and 20:
Background review focused on explic
- Page 21 and 22:
Types of intervention Interventions
- Page 23 and 24:
Box 2.2: Websites searched AFD (Age
- Page 25 and 26:
second stage previously described f
- Page 27 and 28:
using qualitative analysis to attem
- Page 29 and 30:
Figure 3.1: Filtering of papers fro
- Page 31 and 32:
Middle East and North Africa (8%) S
- Page 33 and 34:
Search results access or satisfacti
- Page 35 and 36:
4. Synthesis results Summary Synthe
- Page 37 and 38:
Synthesis results Four studies focu
- Page 39 and 40:
Drug treatments (including micronut
- Page 41 and 42:
Synthesis results Training and audi
- Page 43 and 44:
Synthesis results order to be effec
- Page 45 and 46:
Synthesis results government admini
- Page 47 and 48:
HIV/AIDS and Malaria, as well as no
- Page 49 and 50:
Synthesis results ASSESSING THE COS
- Page 51 and 52:
and birthing care services, includi
- Page 53 and 54:
Synthesis results of settings were
- Page 55 and 56:
Figure 4.1: Causal chain for matern
- Page 57 and 58:
4.3 Summary of results of causal ch
- Page 59 and 60:
5. Strengths and limitations Summar
- Page 61 and 62:
6. Conclusions and recommendations
- Page 63 and 64:
Conclusions and recommendations Urb
- Page 65 and 66:
References Bakr A F, Karkour T (200
- Page 67 and 68:
References Deschamps M M, Noel F, B
- Page 69 and 70:
References Lim S, Dandona L, Hoisin
- Page 71 and 72:
References Shantharam Baliga B, Rag
- Page 73 and 74:
References Channon A A, Falkingham
- Page 75 and 76:
References Jowett M (2000) Safe Mot
- Page 77 and 78:
References Rice J, Rice J S (2009)
- Page 79 and 80:
Appendices Appendix 1.1: Authorship
- Page 81 and 82:
Appendix 2.1: Inclusion and exclusi
- Page 83 and 84:
Appendix 2.2: Search strategy for e
- Page 85 and 86:
Appendix 2.2 Infant* OR Matern* OR
- Page 87 and 88:
OR/ 12-13 11 AND 14 Limit 15 to pub
- Page 89 and 90:
Appendix 2.4: Journals handsearched
- Page 91 and 92:
POOR PROFILE Is the study populatio
- Page 93 and 94:
infants (
- Page 95 and 96:
Appendix 2.5 Intervention (surgical
- Page 97 and 98:
Appendix 2.5 Intervention (service
- Page 99 and 100:
MORTALITY OUTCOME TYPES Which morta
- Page 101 and 102:
positive neutral negative unclear/n
- Page 103 and 104:
yes no unclear/not stated N/A Study
- Page 105 and 106:
surveillance system none of the abo
- Page 107 and 108:
no SELECTION CHARACTERISTICS Is inf
- Page 109 and 110:
Appendix 2.5 QUANTITATIVE DATA ADJU
- Page 111 and 112:
RESEARCHER RELATIONSHIP Has the rel
- Page 113 and 114:
Were the inclusion/exclusion criter
- Page 115 and 116:
person-years). 3.5 Was follow-up ti
- Page 117 and 118:
Appendix 2.7 Appendix 2.7: Quality
- Page 119 and 120:
triangulation, or for not triangula
- Page 121 and 122:
Was the study approved by an ethics
- Page 123 and 124:
Item Yes No Not clear 3. The viewpo
- Page 125 and 126:
Appendix 2.9: Electronic databases
- Page 127 and 128:
Web of Knowledge (including ISI Cit
- Page 129 and 130:
Study Setting Intervention type Abo
- Page 131 and 132:
Study Setting Intervention type Alw
- Page 133 and 134:
Study Setting Intervention type Ben
- Page 135 and 136:
Study Setting Intervention type Ble
- Page 137 and 138:
Study Setting Intervention type Cob
- Page 139 and 140:
Study Setting Intervention type Des
- Page 141 and 142:
Study Setting Intervention type Faw
- Page 143 and 144:
Study Setting Intervention type Jak
- Page 145 and 146:
Study Setting Intervention type Kup
- Page 147 and 148:
Study Setting Intervention type Mar
- Page 149 and 150: Study Setting Intervention type Nah
- Page 151 and 152: Study Setting Intervention type Pad
- Page 153 and 154: Study Setting Intervention type Str
- Page 155 and 156: Study Setting Intervention type Zia
- Page 157 and 158: Appendix 3.2 Adam G K, Abdulla M A,
- Page 159 and 160: Appendix 3.2 Balkus J, Bosire R, Jo
- Page 161 and 162: Appendix 3.2 Boerma J T, Stroh G (1
- Page 163 and 164: Appendix 3.2 Chiwuzie J, Okojie O,
- Page 165 and 166: Appendix 3.2 De Alencar A E, Arraes
- Page 167 and 168: Appendix 3.2 Ekman B, Pathmanathan
- Page 169 and 170: Appendix 3.2 Garg R, Omwomo W, Witt
- Page 171 and 172: Appendix 3.2 Gupta R, Sachdev H P,
- Page 173 and 174: Appendix 3.2 Hutton G, Schellenberg
- Page 175 and 176: Appendix 3.2 Khandker S R, Latif M
- Page 177 and 178: Appendix 3.2 Lindblade K A, Eisele
- Page 179 and 180: Appendix 3.2 Menéndez C, Bardají
- Page 181 and 182: Appendix 3.2 Nduati R, John G, Mbor
- Page 183 and 184: Appendix 3.2 O'Rourke K (1995a) The
- Page 185 and 186: Appendix 3.2 Prual A, De Bernis L,
- Page 187 and 188: Appendix 3.2 Sabitu K, Alti-Mu'azu
- Page 189 and 190: Appendix 3.2 Smith J B, Coleman N A
- Page 191 and 192: Appendix 3.2 Van Rheenen P, De Moor
- Page 193 and 194: Appendix 3.2 Xiang X, Wang L, Xu L
- Page 195 and 196: Appendix 3.4 Appendix 3.4: Studies
- Page 197 and 198: Appendix 3.4 International Bank for
- Page 199: Appendix 3.5 Appendix 3.5: Studies
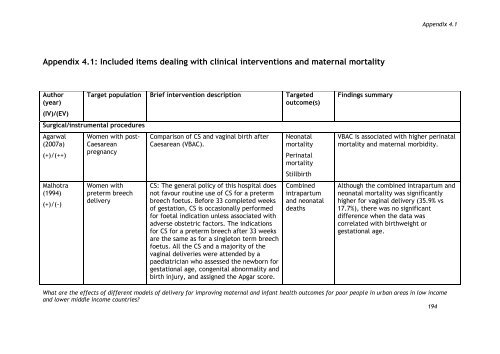
- Page 203 and 204: Chinayon (1998) (+)/(+) Kamilya (20
- Page 205 and 206: Nahar (2004) (-)/(-) Tukur (2007) (
- Page 207 and 208: Ndibazza (2010) (++)/(+) Antiretrov
- Page 209 and 210: Bergstrom (1991) (+)/(+) Women with
- Page 211 and 212: Enakpene (2010) (+)/(-) Etuk (2000a
- Page 213 and 214: Pereira (1996) (-)/(-) Saleem (2007
- Page 215 and 216: Author (year) (IV)/(EV) Joshi (2007
- Page 217 and 218: Author (year) (IV)/(EV) Aaby (2005)
- Page 219 and 220: Author (year) (IV)/(EV) Martins (20
- Page 221 and 222: Author (year) (IV)/(EV) de Muylder
- Page 223 and 224: Author (year) (IV)/(EV) Provider mo
- Page 225 and 226: Appendix 4.4: Included items dealin
- Page 227 and 228: Author (year) (IV)/(EV) Target Popu
- Page 229 and 230: Author (year) (IV)/(EV) Colonna (19
- Page 231 and 232: Author (year) (IV)/(EV) Kuhn (2008)
- Page 233 and 234: Author (year) (IV)/(EV) Target popu
- Page 235 and 236: Author (year) (IV)/(EV) Mswia (2003
- Page 237 and 238: Appendix 4.6: Included items dealin
- Page 239 and 240: Appendix 4.8 Appendix 4.8: Economic
- Page 241 and 242: Author (year) (IV)/(EV) and setting
- Page 243 and 244: Appendix 4.9: Included items identi
- Page 245 and 246: Author (year) (IV)/(EV) Poor urban
- Page 247 and 248: Author (year) (IV)/(EV) Poor urban
- Page 249 and 250: Appendix 4.10: High-quality include
- Page 251:
The authors of this report were sup