Journal Thoracic Oncology
WCLC2016-Abstract-Book_vF-WEB_revNov17-1
WCLC2016-Abstract-Book_vF-WEB_revNov17-1
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
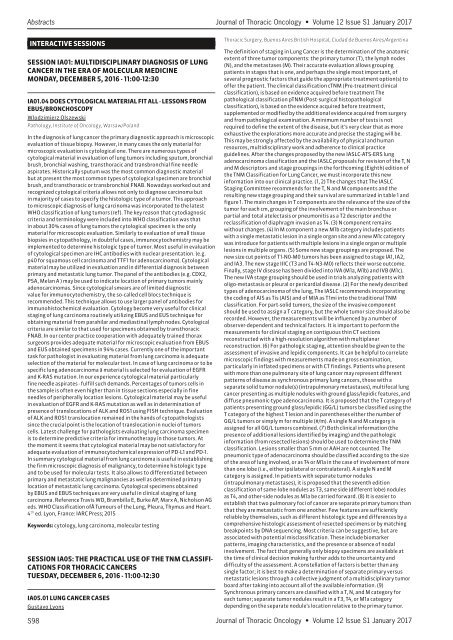
Abstracts <strong>Journal</strong> of <strong>Thoracic</strong> <strong>Oncology</strong> • Volume 12 Issue S1 January 2017<br />
INTERACTIVE SESSIONS<br />
SESSION IA01: MULTIDISCIPLINARY DIAGNOSIS OF LUNG<br />
CANCER IN THE ERA OF MOLECULAR MEDICINE<br />
MONDAY, DECEMBER 5, 2016 - 11:00-12:30<br />
IA01.04 DOES CYTOLOGICAL MATERIAL FIT ALL - LESSONS FROM<br />
EBUS/BRONCHOSCOPY<br />
Wlodzimierz Olszewski<br />
Pathology, Institute of <strong>Oncology</strong>, Warsaw/Poland<br />
In the diagnosis of lung cancer the primary diagnostic approach is microscopic<br />
evaluation of tissue biopsy. However, in many cases the only material for<br />
microscopic evaluation is cytological one. There are numerous types of<br />
cytological material in evaluation of lung tumors including sputum, bronchial<br />
brush, bronchial washing, transthoracic and transbronchial fine needle<br />
aspirates. Historically sputum was the most common diagnostic material<br />
but at present the most common types of cytological specimen are bronchial<br />
brush, and transthoracic or transbronchial FNAB. Nowadays worked out and<br />
recognized cytological criteria allows not only to diagnose carcinoma but<br />
in majority of cases to specify the histologic type of a tumor. This approach<br />
to microscopic diagnosis of lung carcinoma was incorporated to the latest<br />
WHO classification of lung tumors (ref). The key reason that cytodiagnosic<br />
criteria and terminology were included into WHO classification was that<br />
in about 30% cases of lung tumors the cytological specimen is the only<br />
material for microscopic evaluation. Similarly to evaluation of small tissue<br />
biopsies in cytopathology, in doubtful cases, immunocytochemistry may be<br />
implemented to determine histologic type of tumor. Most useful in evaluation<br />
of cytological specimen are IHC antibodies with nuclear presentation. (e.g.<br />
p40 for squamous cell carcinoma and TTF1 for adenocarcinoma). Cytological<br />
material may be utilized in evaluation and in differential diagnosis between<br />
primary and metastatic lung tumor. The panel of the antibodies (e.g. CDX2,<br />
PSA, Melan A ) may be used to indicate location of primary tumors mainly<br />
adenocarcinomas. Since cytological smears are of limited diagnostic<br />
value for immunocytochemistry, the so-called cell blocs technique is<br />
recommended. This technique allows to use larger panel of antibodies for<br />
immunohistochemical evaluation. Cytology become very useful for clinical<br />
staging of lung carcinoma routinely utilizing EBUS and EUS technique for<br />
obtaining material from parahilar and mediastinal lymph nodes. Cytological<br />
criteria are similar to that used for specimens obtained by transthoracic<br />
FNAB. In our center practice cooperation with adequately trained thorax<br />
surgeons provides adequate material for microscopic evaluation from EBUS<br />
and EUS obtained specimens in 94% cases. Currently one of the important<br />
task for pathologist in evaluating material from lung carcinoma is adequate<br />
selection of the material for molecular test. In case of lung carcinoma or to be<br />
specific lung adenocarcinoma â material is selected for evaluation of EGFR<br />
and K-RAS mutation. In our experience cytological material particularly<br />
fine needle aspirates - fulfill such demands. Percentages of tumors cells in<br />
the sample is often even higher than in tissue sections especially in fine<br />
needles of peripherally location lesions. Cytological material may be useful<br />
in evaluation of EGFR and K-RAS mutation as well as in determination of<br />
presence of translocations of ALK and ROS1 using FISH technique. Evaluation<br />
of ALK and ROS1 translocation remained in the hands of cytopathologists<br />
since the crucial point is the location of translocation in nuclei of tumors<br />
cells. Latest challenge for pathologists evaluating lung carcinoma specimen<br />
is to determine predictive criteria for immunotherapy in those tumors. At<br />
the moment it seems that cytological material may be not satisfactory for<br />
adequate evaluation of immunocytochemical expression of PD-L1 and PD-1.<br />
In summary cytological material from lung carcinoma is useful in establishing<br />
the firm microscopic diagnosis of malignancy, to determine histologic type<br />
and to be used for molecular tests. It also allows to differentiated between<br />
primary and metastatic lung malignancies as well as determined primary<br />
location of metastatic lung carcinoma. Cytological specimens obtained<br />
by EBUS and EBUS techniques are very useful in clinical staging of lung<br />
carcinoma. Reference Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG<br />
eds. WHO Classification of Tumours of the Lung, Pleura, Thymus and Heart.<br />
4 th ed. Lyon, France: IARC Press; 2015<br />
Keywords: cytology, lung carcinoma, molecular testing<br />
SESSION IA05: THE PRACTICAL USE OF THE TNM CLASSIFI-<br />
CATIONS FOR THORACIC CANCERS<br />
TUESDAY, DECEMBER 6, 2016 - 11:00-12:30<br />
IA05.01 LUNG CANCER CASES<br />
Gustavo Lyons<br />
<strong>Thoracic</strong> Surgery, Buenos Aires British Hospital, Ciudad de Buenos Aires/Argentina<br />
The definition of staging in Lung Cancer is the determination of the anatomic<br />
extent of three tumor components: the primary tumor (T), the lymph nodes<br />
(N), and the metastases (M). Their accurate evaluation allows grouping<br />
patients in stages that is one, and perhaps the single most important, of<br />
several prognostic factors that guide the appropriate treatment option(s) to<br />
offer the patient. The clinical classification cTNM (Pre-treatment clinical<br />
classification), is based on evidence acquired before treatment The<br />
pathological classification pTNM (Post-surgical histopathological<br />
classification), is based on the evidence acquired before treatment,<br />
supplemented or modified by the additional evidence acquired from surgery<br />
and from pathological examination. A minimum number of tests is not<br />
required to define the extent of the disease, but it’s very clear that as more<br />
exhaustive the explorations more accurate and precise the staging will be.<br />
This may be strongly affected by the availability of physical and human<br />
resources, multidisciplinary work and adherence to clinical practice<br />
guidelines. After the changes proposed by the new IASLC-ATS-ERS lung<br />
adenocarcinoma classification and the IASLC proposals for revision of the T, N<br />
and M descriptors and stage groupings in the forthcoming (Eighth) edition of<br />
the TNM Classification for Lung Cancer, we must incorporate this new<br />
information into our clinical practice. (1, 2) The changes that The IASLC<br />
Staging Committee recommends for the T, N and M components and the<br />
resulting new stage grouping and their survival are summarized in table 1 and<br />
figure 1. The main changes in T components are the relevance of the size of the<br />
tumor for each cm, grouping of the involvement of the main bronchus or<br />
partial and total atelectasis or pneumonitis as a T2 descriptor and the<br />
reclassification of diaphragm invasion as T4. (3) N component remains<br />
without changes. (4) In M component a new M1b category includes patients<br />
with a single metastatic lesion in a single organ site and a new M1c category<br />
was introduce for patients with multiple lesions in a single organ or multiple<br />
lesions in multiple organs. (5) Some new stage groupings are proposed. The<br />
new size cut points of T1-N0-M0 tumors has been assigned to stage IA1, IA2,<br />
and IA3. The new stage IIIC (T3 and T4-N3-M0) reflects their worse outcome.<br />
Finally, stage IV disease has been divided into IVA (M1a, M1b) and IVB (M1c).<br />
The new IVA stage grouping should be used in trials analyzing patients with<br />
oligo-metastasis or pleural or pericardial disease. (2) For the newly described<br />
types of adenocarcinoma of the lung, The IASLC recommends incorporating<br />
the coding of AIS as Tis (AIS) and of MIA as T1mi into the traditional TNM<br />
classification. For part-solid tumors, the size of the invasive component<br />
should be used to assign a T category, but the whole tumor size should also be<br />
recorded. However, the measurements will be influenced by a number of<br />
observer-dependent and technical factors. It is important to perform the<br />
measurements for clinical staging on contiguous thin CT sections<br />
reconstructed with a high-resolution algorithm with multiplanar<br />
reconstruction. (6) For pathologic staging, attention should be given to the<br />
assessment of invasive and lepidic components. It can be helpful to correlate<br />
microscopic findings with measurements made on gross examination,<br />
particularly in inflated specimens or with CT findings. Patients who present<br />
with more than one pulmonary site of lung cancer may represent different<br />
patterns of disease as synchronous primary lung cancers, those with a<br />
separate solid tumor nodule(s) (intrapulmonary metastases), multifocal lung<br />
cancer presenting as multiple nodules with ground glass/lepidic features, and<br />
diffuse pneumonic-type adenocarcinoma. It is proposed that the T category of<br />
patients presenting ground glass/lepidic (GG/L) tumors be classified using the<br />
T category of the highest T lesion and in parentheses either the number of<br />
GG/L tumors or simply m for multiple (#/m). A single N and M category is<br />
assigned for all GG/L tumors combined. (7) Both clinical information (the<br />
presence of additional lesions identified by imaging) and the pathologic<br />
information (from resected lesions) should be used to determine the TNM<br />
classification. Lesions smaller than 5 mm or AAH are not counted. The<br />
pneumonic type of adenocarcinoma should be classified according to the size<br />
of the area of lung involved, or as T4 or M1a in the case of involvement of more<br />
than one lobe (i.e., either ipsilateral or contralateral). A single N and M<br />
category is assigned. In patients with separate tumor nodules<br />
(intrapulmonary metastases), it is proposed that the seventh edition<br />
classification of same-lobe nodules as T3, same side (different lobe) nodules<br />
as T4, and other-side nodules as M1a be carried forward. (8) It is easier to<br />
establish that two pulmonary foci of cancer are separate primary tumors than<br />
that they are metastatic from one another. Few features are sufficiently<br />
reliable by themselves, such as different histologic type and differences by a<br />
comprehensive histologic assessment of resected specimens or by matching<br />
breakpoints by DNA sequencing. Most criteria can be suggestive, but are<br />
associated with potential misclassification. These include biomarker<br />
patterns, imaging characteristics, and the presence or absence of nodal<br />
involvement. The fact that generally only biopsy specimens are available at<br />
the time of clinical decision making further adds to the uncertainty and<br />
difficulty of the assessment. A constellation of factors is better than any<br />
single factor; it is best to make a determination of separate primary versus<br />
metastatic lesions through a collective judgment of a multidisciplinary tumor<br />
board after taking into account all of the available information. (9)<br />
Synchronous primary cancers are classified with a T, N, and M category for<br />
each tumor; separate tumor nodules result in a T3, T4, or M1a category<br />
depending on the separate nodule’s location relative to the primary tumor.<br />
S98 <strong>Journal</strong> of <strong>Thoracic</strong> <strong>Oncology</strong> • Volume 12 Issue S1 January 2017