Is headspace making a difference to young people’s lives?
Evaluation-of-headspace-program
Evaluation-of-headspace-program
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
5. Service Delivery Model<br />
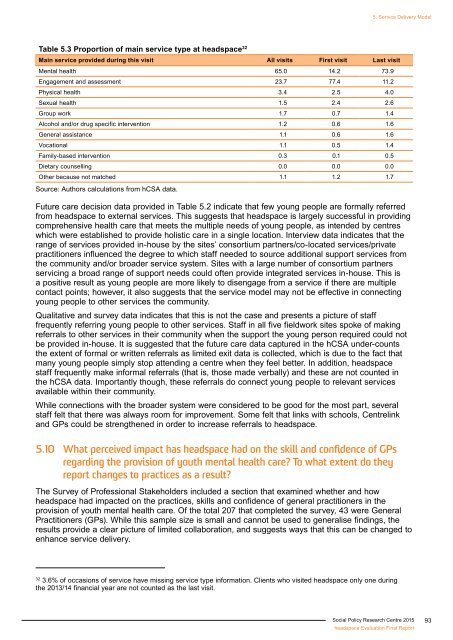
Table 5.3 Proportion of main service type at <strong>headspace</strong> 32<br />
Main service provided during this visit All visits First visit Last visit<br />
Mental health 65.0 14.2 73.9<br />
Engagement and assessment 23.7 77.4 11.2<br />
Physical health 3.4 2.5 4.0<br />
Sexual health 1.5 2.4 2.6<br />
Group work 1.7 0.7 1.4<br />
Alcohol and/or drug specific intervention 1.2 0.6 1.6<br />
General assistance 1.1 0.6 1.6<br />
Vocational 1.1 0.5 1.4<br />
Family-based intervention 0.3 0.1 0.5<br />
Dietary counselling 0.0 0.0 0.0<br />
Other because not matched 1.1 1.2 1.7<br />
Source: Authors calculations from hCSA data.<br />
Future care decision data provided in Table 5.2 indicate that few <strong>young</strong> people are formally referred<br />
from <strong>headspace</strong> <strong>to</strong> external services. This suggests that <strong>headspace</strong> is largely successful in providing<br />
comprehensive health care that meets the multiple needs of <strong>young</strong> people, as intended by centres<br />
which were established <strong>to</strong> provide holistic care in a single location. Interview data indicates that the<br />
range of services provided in-house by the sites’ consortium partners/co-located services/private<br />
practitioners influenced the degree <strong>to</strong> which staff needed <strong>to</strong> source additional support services from<br />
the community and/or broader service system. Sites with a large number of consortium partners<br />
servicing a broad range of support needs could often provide integrated services in-house. This is<br />
a positive result as <strong>young</strong> people are more likely <strong>to</strong> disengage from a service if there are multiple<br />
contact points; however, it also suggests that the service model may not be effective in connecting<br />
<strong>young</strong> people <strong>to</strong> other services the community.<br />
Qualitative and survey data indicates that this is not the case and presents a picture of staff<br />
frequently referring <strong>young</strong> people <strong>to</strong> other services. Staff in all five fieldwork sites spoke of <strong>making</strong><br />
referrals <strong>to</strong> other services in their community when the support the <strong>young</strong> person required could not<br />
be provided in-house. It is suggested that the future care data captured in the hCSA under-counts<br />
the extent of formal or written referrals as limited exit data is collected, which is due <strong>to</strong> the fact that<br />
many <strong>young</strong> people simply s<strong>to</strong>p attending a centre when they feel better. In addition, <strong>headspace</strong><br />
staff frequently make informal referrals (that is, those made verbally) and these are not counted in<br />
the hCSA data. Importantly though, these referrals do connect <strong>young</strong> people <strong>to</strong> relevant services<br />
available within their community.<br />
While connections with the broader system were considered <strong>to</strong> be good for the most part, several<br />
staff felt that there was always room for improvement. Some felt that links with schools, Centrelink<br />
and GPs could be strengthened in order <strong>to</strong> increase referrals <strong>to</strong> <strong>headspace</strong>.<br />
5.10 What perceived impact has <strong>headspace</strong> had on the skill and confidence of GPs<br />
regarding the provision of youth mental health care? To what extent do they<br />
report changes <strong>to</strong> practices as a result?<br />
The Survey of Professional Stakeholders included a section that examined whether and how<br />
<strong>headspace</strong> had impacted on the practices, skills and confidence of general practitioners in the<br />
provision of youth mental health care. Of the <strong>to</strong>tal 207 that completed the survey, 43 were General<br />
Practitioners (GPs). While this sample size is small and cannot be used <strong>to</strong> generalise findings, the<br />
results provide a clear picture of limited collaboration, and suggests ways that this can be changed <strong>to</strong><br />
enhance service delivery.<br />
32<br />
3.6% of occasions of service have missing service type information. Clients who visited <strong>headspace</strong> only one during<br />
the 2013/14 financial year are not counted as the last visit.<br />
Social Policy Research Centre 2015<br />
<strong>headspace</strong> Evaluation Final Report<br />
93