Is headspace making a difference to young people’s lives?
Evaluation-of-headspace-program
Evaluation-of-headspace-program
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
5. Service Delivery Model<br />
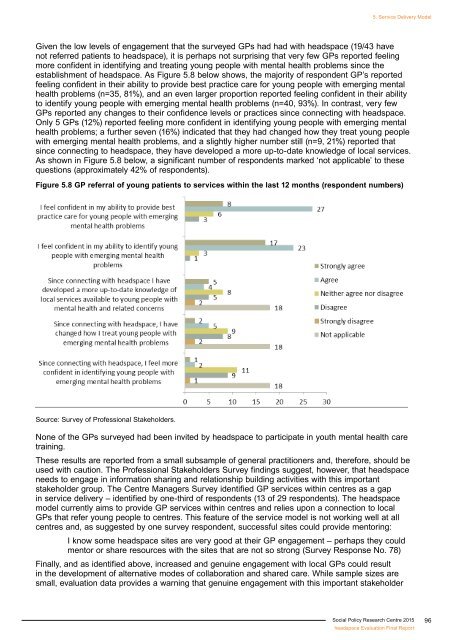
Given the low levels of engagement that the surveyed GPs had had with <strong>headspace</strong> (19/43 have<br />
not referred patients <strong>to</strong> <strong>headspace</strong>), it is perhaps not surprising that very few GPs reported feeling<br />
more confident in identifying and treating <strong>young</strong> people with mental health problems since the<br />
establishment of <strong>headspace</strong>. As Figure 5.8 below shows, the majority of respondent GP’s reported<br />
feeling confident in their ability <strong>to</strong> provide best practice care for <strong>young</strong> people with emerging mental<br />
health problems (n=35, 81%), and an even larger proportion reported feeling confident in their ability<br />
<strong>to</strong> identify <strong>young</strong> people with emerging mental health problems (n=40, 93%). In contrast, very few<br />
GPs reported any changes <strong>to</strong> their confidence levels or practices since connecting with <strong>headspace</strong>.<br />
Only 5 GPs (12%) reported feeling more confident in identifying <strong>young</strong> people with emerging mental<br />
health problems; a further seven (16%) indicated that they had changed how they treat <strong>young</strong> people<br />
with emerging mental health problems, and a slightly higher number still (n=9, 21%) reported that<br />
since connecting <strong>to</strong> <strong>headspace</strong>, they have developed a more up-<strong>to</strong>-date knowledge of local services.<br />
As shown in Figure 5.8 below, a significant number of respondents marked ‘not applicable’ <strong>to</strong> these<br />
questions (approximately 42% of respondents).<br />
Figure 5.8 GP referral of <strong>young</strong> patients <strong>to</strong> services within the last 12 months (respondent numbers)<br />
Source: Survey of Professional Stakeholders.<br />
None of the GPs surveyed had been invited by <strong>headspace</strong> <strong>to</strong> participate in youth mental health care<br />
training.<br />
These results are reported from a small subsample of general practitioners and, therefore, should be<br />
used with caution. The Professional Stakeholders Survey findings suggest, however, that <strong>headspace</strong><br />
needs <strong>to</strong> engage in information sharing and relationship building activities with this important<br />
stakeholder group. The Centre Managers Survey identified GP services within centres as a gap<br />
in service delivery – identified by one-third of respondents (13 of 29 respondents). The <strong>headspace</strong><br />
model currently aims <strong>to</strong> provide GP services within centres and relies upon a connection <strong>to</strong> local<br />
GPs that refer <strong>young</strong> people <strong>to</strong> centres. This feature of the service model is not working well at all<br />
centres and, as suggested by one survey respondent, successful sites could provide men<strong>to</strong>ring:<br />
I know some <strong>headspace</strong> sites are very good at their GP engagement – perhaps they could<br />
men<strong>to</strong>r or share resources with the sites that are not so strong (Survey Response No. 78)<br />
Finally, and as identified above, increased and genuine engagement with local GPs could result<br />
in the development of alternative modes of collaboration and shared care. While sample sizes are<br />
small, evaluation data provides a warning that genuine engagement with this important stakeholder<br />
Social Policy Research Centre 2015<br />
<strong>headspace</strong> Evaluation Final Report<br />
96