Protocols - Hemorio
Protocols - Hemorio
Protocols - Hemorio
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Each dose corresponds to a unit of CP obtained from a unit of whole blood / 10 kg of weight from the<br />
receptor or a unit of CP obtained by apheresis.<br />
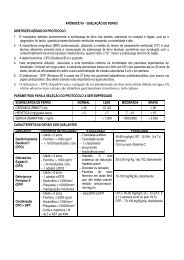
DOSES AND ADMINISTRATION INTERVALS<br />
Prophylactic Transfusion: The dosage used must be 1 unit (or 5.5 X 10 10 platelets) for every 7-10 Kg of<br />
subject’s weight. In children with a weight below 7 Kg, the dosage must be 10 to 15 ml/Kg. However,<br />
lowest doses, of at least a unit for every 5 Kg of the subject’s weight, can be accepted. Most of the times,<br />
the prophylactic transfusion needs to be repeated every 24 to 48 hours.<br />
Therapeutic Transfusion: The purpose of the therapeutic transfusion of platelets is not to increase the<br />
platelets counting above certain limit, but to help correcting the hemostatic disturbance, that might be<br />
contributing to the hemorrhage.<br />
The dosage at the curative transfusion is 1 unit for every 7 kg of weight, and the intervals of administration<br />
are shorter (8 to 12 hours), until the hemorrhage is controlled.<br />
The therapeutic transfusion of platelets is indicated for the subject that presents platelet dysfunction and<br />
life-threatening hemorrhage, regardless the platelets counting.<br />
The therapeutic transfusion of platelets is also indicated for the subject that presents ongoing hemorrhage<br />
and platelets counting below 50,000/µL.<br />
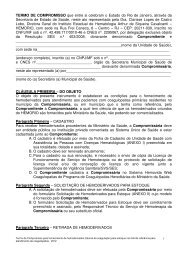
ABO-COMPATIBILITY AND Rh:<br />
ABO-incompatible platelets transfusions are not contraindicated, although the ideal is always the<br />
ABO-compatible platelets transfusion. When the platelets concentrates are roughly contaminated by<br />
red blood cells, no ABO-incompatible platelets must be transfused.<br />
The negative Rh subjects must only receive negative Rh platelets. If it is not possible, and if positive Rh<br />
platelets must be used in negative Rh subjects, it is recommended the usage of anti-D immunoglobulin up<br />
to 72 hours, after the transfusion, in order to prevent the sensitivity of the subject. This recommendation<br />
must be strictly followed in female children and child-bearing potential women.<br />
If the subject needs to be transfused again, the infusion of anti-D must be repeated only when the residual<br />
pre-transfusional anti-D research is negative.<br />
DE-LEUKOCYTATION OF PLATELETS: All platelets transfusions must be done, whenever possible, with<br />
de-leukocytated platelets.<br />
THROMBOCYTOPENIA AND ANEMIA: It is recommended that the dosage of hemoglobin in subjects<br />
with post-chemotherapy thrombocytopenia is kept above 8g%. This recommendation is also applied to the<br />
subjects refractory to the platelets transfusion for which no HLA-compatible platelets can be provided.<br />
APLASIA OF POST-QT AND/OR RXT MARROW (INCLUDING TMO), APLASTIC ANEMIA AND MDS:<br />
The transfusion is indicated when there are hemorrhages other than petechia, ecchymosis and<br />
gingivorrhage, and the platelets counting is below 50,000/µL. Among the hemorrhages that require the<br />
curative transfusion, the hemorrhagic blisters are included.<br />
163