- Page 3 and 4:
Attachment I Special Term and Condi
- Page 5 and 6:
Attachment II Special Term and Cond
- Page 7 and 8: RICK SCOTT GOVERNOR 272 7 Mah an Dr
- Page 9 and 10: • Encounter data • Systems issu
- Page 11 and 12: Appendix A How to Become a Florida
- Page 13 and 14: How to Become a Florida Medicaid He
- Page 15 and 16: Appendix B MCO Application Checklis
- Page 17 and 18: 4 5 6 7 8 9 10 Service Level(s) are
- Page 19 and 20: 19 b. Total number of employees; AP
- Page 21 and 22: APPLICATION ITEM 25 3. In the past
- Page 23 and 24: 32 33 34 35 36 APPLICATION ITEM 10.
- Page 25 and 26: APPLICATION ITEM C. Criminal Backgr
- Page 27 and 28: APPLICATION ITEM 43 13. For medical
- Page 29 and 30: 46 47 APPLICATION ITEM 16. Indicate
- Page 31 and 32: 49 APPLICATION ITEM 19. Describe in
- Page 33 and 34: 51 52 53 54 55 56 APPLICATION ITEM
- Page 35 and 36: Attachment III Special Term and Con
- Page 37 and 38: RICK SCOTT GOVERNOR Regulatory Auth
- Page 39 and 40: e. Complete a credentialing review
- Page 41 and 42: RICK SCOTT GOVERNOR Regulatory Auth
- Page 43 and 44: Compliance Monitoring Tool with Spe
- Page 45 and 46: Standard I: Care Management/Continu
- Page 47 and 48: Standard I: Care Management/Continu
- Page 49 and 50: Standard I: Care Management/Continu
- Page 51 and 52: Results for Standard I Care Managem
- Page 53 and 54: Standarrd II: Utilizatio on Managem
- Page 55 and 56: Standarrd II: Utilizatio on Managem
- Page 57: Standarrd II: Utilizatio on Managem
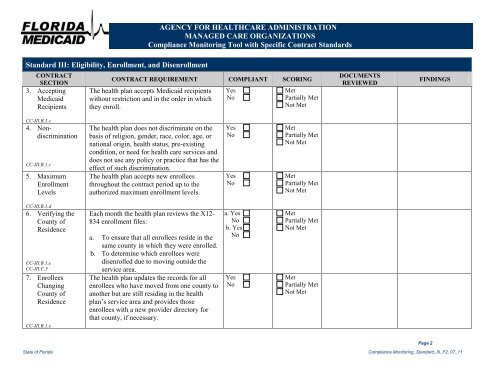
- Page 61 and 62: Standard III: Eligibility, Enrollme
- Page 63 and 64: Standard III: Eligibility, Enrollme
- Page 65 and 66: Standard III: Eligibility, Enrollme
- Page 67 and 68: Standard III: Eligibility, Enrollme
- Page 69 and 70: Standard III: Eligibility, Enrollme
- Page 71 and 72: Standard III: Eligibility, Enrollme
- Page 73 and 74: Standard III: Eligibility, Enrollme
- Page 75 and 76: Standard III: Eligibility, Enrollme
- Page 77 and 78: Standard IV: Enrollee Services & En
- Page 79 and 80: Standard IV: Enrollee Services & En
- Page 81 and 82: Standard IV: Enrollee Services & En
- Page 83 and 84: Standard IV: Enrollee Services & En
- Page 85 and 86: Standard IV: Enrollee Services & En
- Page 87 and 88: Standard IV: Enrollee Services & En
- Page 89 and 90: Standard IV: Enrollee Services & En
- Page 91 and 92: Standard IV: Enrollee Services & En
- Page 93 and 94: Standard IV: Enrollee Services & En
- Page 95 and 96: Standard IV: Enrollee Services & En
- Page 97 and 98: Standard IV: Enrollee Services & En
- Page 99 and 100: Standard IV: Enrollee Services & En
- Page 101 and 102: Standard IV: Enrollee Services & En
- Page 103 and 104: Results for Standard IV Enrollee Se
- Page 105 and 106: Standard V: Provider Credentialing
- Page 107 and 108: Standard VI: Provider Services CONT
- Page 109 and 110:
Standard VI: Provider Services CC-
- Page 111 and 112:
Standard VI: Provider Services CONT
- Page 113 and 114:
Standard VII: Provider Contracting
- Page 115 and 116:
AGENCY FOR HEALTHCARE ADMINISTRATIO
- Page 117 and 118:
Standard VIII: Quality Improvement
- Page 119 and 120:
Standard VIII: Quality Improvement
- Page 121 and 122:
Standard VIII: Quality Improvement
- Page 123 and 124:
Standard VIII: Quality Improvement
- Page 125 and 126:
Standard VIII: Quality Improvement
- Page 127 and 128:
AGENCY FOR HEALTHCARE ADMINISTRATIO
- Page 129 and 130:
Results for Standard IX Medical Rec
- Page 131 and 132:
Standard X: Access and Availability
- Page 133 and 134:
Standard X: Access and Availability
- Page 135 and 136:
Standard X: Access and Availability
- Page 137 and 138:
Standard X: Access and Availability
- Page 139 and 140:
Standard X: Access and Availability
- Page 141 and 142:
Standard X: Access and Availability
- Page 143 and 144:
Standard X: Access and Availability
- Page 145 and 146:
Results for Standard X Access and A
- Page 147 and 148:
Standard XI: Grievances and Appeals
- Page 149 and 150:
Standard XI: Grievances and Appeals
- Page 151 and 152:
Standard XI: Grievances and Appeals
- Page 153 and 154:
Standard XI: Grievances and Appeals
- Page 155 and 156:
Standard XI: Grievances and Appeals
- Page 157 and 158:
Standard XI: Grievances and Appeals
- Page 159 and 160:
Standard XI: Grievances and Appeals
- Page 161 and 162:
AGENCY FOR HEALTHCARE ADMINISTRATIO
- Page 163 and 164:
Standard XII: Administration and Ma
- Page 165 and 166:
Standard XII: Administration and Ma
- Page 167 and 168:
Standard XII: Administration and Ma
- Page 169 and 170:
Standard XII: Administration and Ma
- Page 171 and 172:
AGENCY FOR HEALTHCARE ADMINISTRATIO
- Page 173 and 174:
Standard XII: Administration and Ma
- Page 175 and 176:
Standard XII: Administration and Ma
- Page 177 and 178:
Standard XII: Administration and Ma
- Page 179 and 180:
Standard XII: Administration and Ma
- Page 181 and 182:
Standard XII: Administration and Ma
- Page 183 and 184:
Standard XII: Administration and Ma
- Page 185 and 186:
Standard XII: Administration and Ma
- Page 187 and 188:
Standard XII: Administration and Ma
- Page 189 and 190:
Results for Standard XII Administra
- Page 191 and 192:
Standard XIII: Community Outreach C
- Page 193 and 194:
Standard XIII: Community Outreach C
- Page 195 and 196:
Standard XIII: Community Outreach C
- Page 197 and 198:
Standard XIII: Community Outreach C
- Page 199 and 200:
Standard XIII: Community Outreach C
- Page 201 and 202:
Standard XIII: Community Outreach C
- Page 203 and 204:
Results for Standard XIII Community
- Page 205 and 206:
Standard XIV: Covered Services AGEN
- Page 207 and 208:
Standard XIV: Covered Services AGEN
- Page 209 and 210:
Standard XIV: Covered Services AGEN
- Page 211 and 212:
Standard XIV: Covered Services AGEN
- Page 213 and 214:
Standard XIV: Covered Services AGEN
- Page 215 and 216:
Standard XIV: Covered Services AGEN
- Page 217 and 218:
Standard XIV: Covered Services AGEN
- Page 219 and 220:
Standard XIV: Covered Services AGEN
- Page 221 and 222:
Standard XIV: Covered Services AGEN
- Page 223 and 224:
Standard XIV: Covered Services AGEN
- Page 225 and 226:
Standard XIV: Covered Services AGEN
- Page 227 and 228:
Standard XIV: Covered Services AGEN
- Page 229 and 230:
Standard XIV: Covered Services AGEN
- Page 231 and 232:
Standard XIV: Covered Services AGEN
- Page 233 and 234:
Standard XV: Immunizations, Pregnan
- Page 235 and 236:
Standard XV: Immunizations, Pregnan
- Page 237 and 238:
Standard XV: Immunizations, Pregnan
- Page 239 and 240:
Standard XV: Immunizations, Pregnan
- Page 241 and 242:
Standard XV: Immunizations, Pregnan
- Page 243 and 244:
Standard XV: Immunizations, Pregnan
- Page 245 and 246:
Standard XV: Immunizations, Pregnan
- Page 247 and 248:
Standard XV: Immunizations, Pregnan
- Page 249 and 250:
Vendor Name: Review Period: Date of
- Page 251 and 252:
Vendor Name: Review Period: Date of
- Page 253 and 254:
Agency For Health Care Administrati
- Page 255 and 256:
File # Case ID # Agency For Health
- Page 257 and 258:
File # Case ID # 1 2 3 4 5 6 7 8 9
- Page 259 and 260:
Agency For Health Care Administrati
- Page 261 and 262:
13 14 15 Agency For Health Care Adm
- Page 263 and 264:
Agency For Health Care Administrati
- Page 265 and 266:
f. Posting of the Agency Summary of
- Page 267 and 268:
Name: Review Period: Date of Review
- Page 269 and 270:
File # Case ID # Agency For Health
- Page 271 and 272:
File # Case ID # Agency For Health
- Page 273 and 274:
Agency For Health Care Administrati
- Page 275 and 276:
Vendor Name: Review Period: Date of
- Page 277 and 278:
Vendor Name: Review Period: Date of
- Page 279 and 280:
Vendor Name: Review Period: Date of
- Page 281 and 282:
Agency For Health Care Administrati
- Page 283 and 284:
5. 6. 7. 8. 9. local WIC office to
- Page 285 and 286:
Agency For Health Care Administrati
- Page 287 and 288:
Agency For Health Care Administrati
- Page 289 and 290:
14 Agency For Health Care Administr
- Page 291 and 292:
Agency For Health Care Administrati
- Page 293 and 294:
Vendor Name: Review Period: Date of
- Page 295 and 296:
8 providers Agency For Health Care
- Page 297 and 298:
Agency For Health Care Administrati
- Page 299 and 300:
Agency For Health Care Administrati
- Page 301 and 302:
Agency For Health Care Administrati
- Page 303 and 304:
Agency For Health Care Administrati
- Page 305 and 306:
Vendor Name: Review Period: Date of
- Page 307 and 308:
Agency For Health Care Administrati
- Page 309 and 310:
Agency For Health Care Administrati
- Page 311 and 312:
Agency For Health Care Administrati
- Page 313 and 314:
Agency For Health Care Administrati
- Page 315 and 316:
Agency For Health Care Administrati
- Page 317 and 318:
Vendor Name: Review Period: Date of
- Page 319 and 320:
Agency For Health Care Administrati
- Page 321 and 322:
Agency For Health Care Administrati
- Page 323 and 324:
Agency For Health Care Administrati
- Page 325 and 326:
Agency For Health Care Administrati
- Page 327 and 328:
Agency For Health Care Administrati
- Page 329 and 330:
Medical Loss Ratio The following dr
- Page 331 and 332:
RICK SCOTT GOVERNOR Better Health C
- Page 333 and 334:
Plan Name: AGENCY FOR HEALTH CARE A
- Page 335 and 336:
DRAFT ATTESTATION OF 201_ QUARTER E
- Page 337 and 338:
Draft MLR Reporting Schedule Health
- Page 339 and 340:
RICK SCOTT GOVERNOR PLAN TYPES: Bet
- Page 341 and 342:
Attachment V Special Term and Condi
- Page 343 and 344:
RICK SCOTT GOVERNOR Mission to Ensu
- Page 345 and 346:
• Obtaining data from the health
- Page 347 and 348:
RICK SCOTT GOVERNOR Mission to Ensu
- Page 349 and 350:
Attachment VI Special Term and Cond
- Page 351 and 352:
RICK SCOTT GOVERNOR Better Health C