here - Australian College of Veterinary Scientists
here - Australian College of Veterinary Scientists
here - Australian College of Veterinary Scientists
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
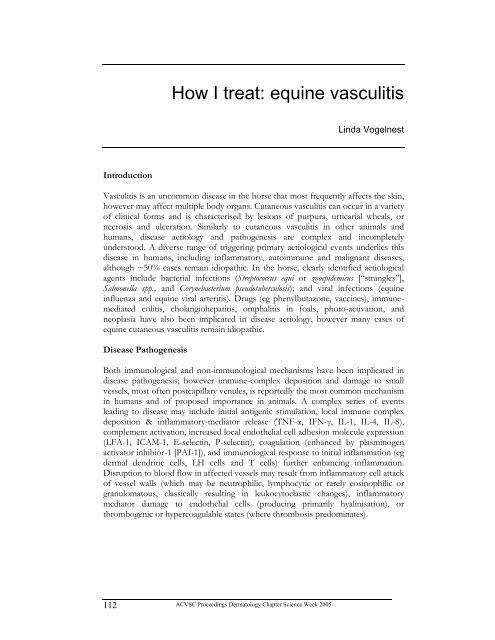
Introduction<br />
112<br />
How I treat: equine vasculitis<br />
ACVSC Proceedings Dermatology Chapter Science Week 2005<br />
Linda Vogelnest<br />
Vasculitis is an uncommon disease in the horse that most frequently affects the skin,<br />
however may affect multiple body organs. Cutaneous vasculitis can occur in a variety<br />
<strong>of</strong> clinical forms and is characterised by lesions <strong>of</strong> purpura, urticarial wheals, or<br />
necrosis and ulceration. Similarly to cutaneous vasculitis in other animals and<br />
humans, disease aetiology and pathogenesis are complex and incompletely<br />
understood. A diverse range <strong>of</strong> triggering primary aetiological events underlies this<br />
disease in humans, including inflammatory, autoimmune and malignant diseases,<br />
although ~50% cases remain idiopathic. In the horse, clearly identified aetiological<br />
agents include bacterial infections (Streptococcus equi or zooepidemicus [“strangles”],<br />
Salmonella spp., and Corynebacterium pseudotuberculosis); and viral infections (equine<br />
influenza and equine viral arteritis). Drugs (eg phenylbutazone, vaccines), immunemediated<br />
colitis, cholangiohepatitis, omphalitis in foals, photo-activation, and<br />
neoplasia have also been implicated in disease aetiology, however many cases <strong>of</strong><br />
equine cutaneous vasculitis remain idiopathic.<br />
Disease Pathogenesis<br />
Both immunological and non-immunological mechanisms have been implicated in<br />
disease pathogenesis; however immune-complex deposition and damage to small<br />
vessels, most <strong>of</strong>ten postcapillary venules, is reportedly the most common mechanism<br />
in humans and <strong>of</strong> proposed importance in animals. A complex series <strong>of</strong> events<br />
leading to disease may include initial antigenic stimulation, local immune complex<br />
deposition & inflammatory-mediator release (TNF-α, IFN-γ, IL-1, IL-4, IL-8),<br />
complement activation, increased local endothelial cell adhesion molecule expression<br />
(LFA-1, ICAM-1, E-selectin, P-selectin), coagulation (enhanced by plasminogen<br />
activator inhibior-1 [PAI-1]), and immunological response to initial inflammation (eg<br />
dermal dendritic cells, LH cells and T cells) further enhancing inflammation.<br />
Disruption to blood flow in affected vessels may result from inflammatory cell attack<br />
<strong>of</strong> vessel walls (which may be neutrophilic, lymphocytic or rarely eosinophilic or<br />
granulomatous, classically resulting in leukocytoclastic changes), inflammatory<br />
mediator damage to endothelial cells (producing primarily hyalinisation), or<br />
thrombogenic or hypercoagulable states (w<strong>here</strong> thrombosis predominates).