Transdermal Diagnosis of MalariaUsing Vapor NanobubblesEkaterina Lukianova-Hleb, Sarah Bezek, Reka Szigeti, Alexander Khodarev, Thomas Kelley,Andrew Hurrell, Michail Berba, Nirbhay Kumar, Umberto D’Alessandro, Dmitri LapotkoA fast, precise, noninvasive, high-throughput, and simpleapproach for detecting malaria in humans and mosquitoesis not possible with current techniques that depend on bloodsampling, reagents, facilities, tedious procedures, andtrained personnel. We designed a device for rapid (20-second)noninvasive diagnosis of Plasmodium falciparum infectionin a malaria patient without drawing blood or usingany reagent. This method uses transdermal optical excitationand acoustic detection of vapor nanobubbles aroundintraparasite hemozoin. The same device also identified individualmalaria parasite–infected Anopheles mosquitoes ina few seconds and can be realized as a low-cost universaltool for clinical and field diagnoses.Malaria control and elimination would benefit greatlyfrom an efficient and universal diagnostic tool thatis fast (provides results in seconds), noninvasive and safe(uses no blood sampling or reagents), simple to use (can beoperated by nonmedical personnel), sensitive and specific(detects low-level asymptomatic infections), and inexpensiveand that detects malarial infection in humans and inmosquitoes (1–21). We recently proposed a transdermalblood- and reagent-free approach based on hemozoin-generatedvapor nanobubbles (H-VNBs) (22) in which malariaparasite–specific endogenous nanocrystals of hemozoin areoptically excited in vivo with a safe and short laser pulse(delivered to blood vessels through the skin). The light isconverted into nonstationary localized heat that evaporatesthe adjacent nanovolume of liquid and thus generates anexpanding and collapsing vapor nanobubble inside the parasite.The nanosize and high optical absorbance of hemozoinprovide higher malaria infection specificity of theseAuthor affiliations: Rice University, Houston, Texas, USA(E. Lukianova-Hleb, D. Lapotko); Baylor College of Medicine,Houston (S. Bezek, R. Szigeti); Ben Taub General Hospital,Houston (S. Bezek, R. Szigeti); X Instruments LLC, Fremont,California, USA (A. Khodarev); Precision Acoustics Ltd, Dorset,UK (T. Kelley, A. Hurrell); Standa UAB, Vilnius, Lithuania(M. Berba); Tulane University, New Orleans, Louisiana, USA(N. Kumar); Medical Research Council, Banjul, The Gambia(U. D’Alessandro); London School of Hygiene and TropicalMedicine, London, UK (U. D’Alessandro)DOI: http://dx.doi.org/10.3201/eid2107.150089H-VNBs than does any normal blood and tissue components(23–26). Their transient expansion and collapse result in anoninvasive pressure pulse that is easily detected throughthe skin with an ultrasound sensor. In our preliminary studies(22), H-VNBs detected parasitemia as low as 0.0001%in vitro (human blood), and 0.00034% in vivo (transdermaldetection in animals), with no false-positive signals.Therefore, H-VNB might be able to detect extremely lowparasite densities provided the method can be applied tohumans or mosquitoes simply and inexpensively.To determine the technical and medical feasibility ofH-VNBs for malaria diagnosis and screening, we prototypeda diagnostic device and evaluated it in a patient withconfirmed malaria and in noninfected persons as controls.We also evaluated the device in Plasmodium falciparum–infected mosquitoes.Materials and MethodsPrototype Design and AlgorithmsThe laboratory prototype (Figure 1, panel A) comprisedthe newly designed compact low-cost pulsed laser (532nm, 10 μJ, 200 ps; Standa, Vilnius, Lithuania). The laserpulse is delivered to the skin by the combination probeat the fluence 36 mJ/cm 2 (Figure 1, panel B). The probewas developed for transdermal diagnostics and includesan optical fiber guide and a custom acoustic sensor witha preamplifier that is integrated in 1 compact hand-heldunit. In response to each laser pulse, the probe detects anacoustic pulse and generates an output electrical signal asan acoustic trace (Figure 1). Its output signals were collectedand analyzed with custom-designed software (NILabVIEW, Austin, TX, USA) by using a signal amplifier,digital oscilloscope (LeCroy 42X; Teledyne LeCroy, NY,USA), and computer. The peak-to-peak amplitude A of theacoustic trace obtained in response to each laser pulse wasmeasured and presented as a histogram for 400 sequentiallaser pulses. A malarial infection–negative trace histogramwas used to determine “the malaria threshold” T as themaximum amplitude for the malarial infection–negativesignal. Any trace with an amplitude above that thresholdwas considered to be hemozoin (malarial infection)–positive.To quantify the infection, we counted the incidencerate of malarial infection–positive traces IR (the probability1122 Emerging Infectious Diseases • www.cdc.gov/eid • Vol. 21, No. 7, July 2015
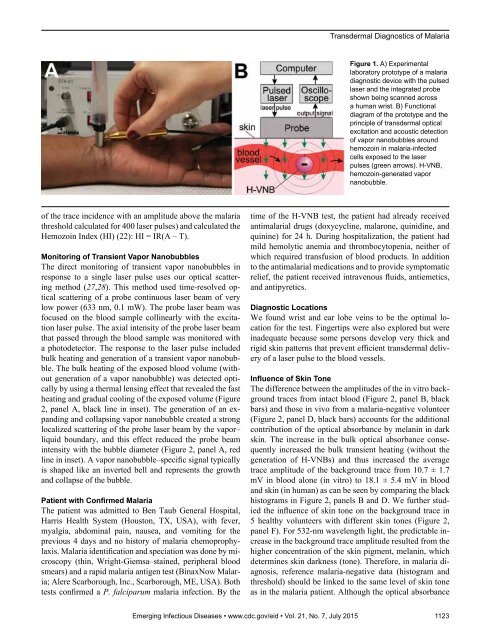
Transdermal Diagnostics of MalariaFigure 1. A) Experimentallaboratory prototype of a malariadiagnostic device with the pulsedlaser and the integrated probeshown being scanned acrossa human wrist. B) Functionaldiagram of the prototype and theprinciple of transdermal opticalexcitation and acoustic detectionof vapor nanobubbles aroundhemozoin in malaria-infectedcells exposed to the laserpulses (green arrows). H-VNB,hemozoin-generated vapornanobubble.of the trace incidence with an amplitude above the malariathreshold calculated for 400 laser pulses) and calculated theHemozoin Index (HI) (22): HI = IR(A – T).Monitoring of Transient Vapor NanobubblesThe direct monitoring of transient vapor nanobubbles inresponse to a single laser pulse uses our optical scatteringmethod (27,28). This method used time-resolved opticalscattering of a probe continuous laser beam of verylow power (633 nm, 0.1 mW). The probe laser beam wasfocused on the blood sample collinearly with the excitationlaser pulse. The axial intensity of the probe laser beamthat passed through the blood sample was monitored witha photodetector. The response to the laser pulse includedbulk heating and generation of a transient vapor nanobubble.The bulk heating of the exposed blood volume (withoutgeneration of a vapor nanobubble) was detected opticallyby using a thermal lensing effect that revealed the fastheating and gradual cooling of the exposed volume (Figure2, panel A, black line in inset). The generation of an expandingand collapsing vapor nanobubble created a stronglocalized scattering of the probe laser beam by the vapor–liquid boundary, and this effect reduced the probe beamintensity with the bubble diameter (Figure 2, panel A, redline in inset). A vapor nanobubble–specific signal typicallyis shaped like an inverted bell and represents the growthand collapse of the bubble.Patient with Confirmed MalariaThe patient was admitted to Ben Taub General Hospital,Harris Health System (Houston, TX, USA), with fever,myalgia, abdominal pain, nausea, and vomiting for theprevious 4 days and no history of malaria chemoprophylaxis.Malaria identification and speciation was done by microscopy(thin, Wright-Giemsa–stained, peripheral bloodsmears) and a rapid malaria antigen test (BinaxNow Malaria;Alere Scarborough, Inc., Scarborough, ME, USA). Bothtests confirmed a P. falciparum malaria infection. By thetime of the H-VNB test, the patient had already receivedantimalarial drugs (doxycycline, malarone, quinidine, andquinine) for 24 h. During hospitalization, the patient hadmild hemolytic anemia and thrombocytopenia, neither ofwhich required transfusion of blood products. In additionto the antimalarial medications and to provide symptomaticrelief, the patient received intravenous fluids, antiemetics,and antipyretics.Diagnostic LocationsWe found wrist and ear lobe veins to be the optimal locationfor the test. Fingertips were also explored but wereinadequate because some persons develop very thick andrigid skin patterns that prevent efficient transdermal deliveryof a laser pulse to the blood vessels.Influence of Skin ToneThe difference between the amplitudes of the in vitro backgroundtraces from intact blood (Figure 2, panel B, blackbars) and those in vivo from a malaria-negative volunteer(Figure 2, panel D, black bars) accounts for the additionalcontribution of the optical absorbance by melanin in darkskin. The increase in the bulk optical absorbance consequentlyincreased the bulk transient heating (without thegeneration of H-VNBs) and thus increased the averagetrace amplitude of the background trace from 10.7 ± 1.7mV in blood alone (in vitro) to 18.1 ± 5.4 mV in bloodand skin (in human) as can be seen by comparing the blackhistograms in Figure 2, panels B and D. We further studiedthe influence of skin tone on the background trace in5 healthy volunteers with different skin tones (Figure 2,panel F). For 532-nm wavelength light, the predictable increasein the background trace amplitude resulted from thehigher concentration of the skin pigment, melanin, whichdetermines skin darkness (tone). Therefore, in malaria diagnosis,reference malaria-negative data (histogram andthreshold) should be linked to the same level of skin toneas in the malaria patient. Although the optical absorbanceEmerging Infectious Diseases • www.cdc.gov/eid • Vol. 21, No. 7, July 2015 1123
- Page 3 and 4: July 2015SynopsisOn the CoverMarian
- Page 5 and 6: 1240 Gastroenteritis OutbreaksCause
- Page 7 and 8: SYNOPSISDisseminated Infections wit
- Page 9 and 10: Disseminated Infections with Talaro
- Page 11 and 12: Disseminated Infections with Talaro
- Page 13 and 14: Macacine Herpesvirus 1 inLong-Taile
- Page 15 and 16: Macacine Herpesvirus 1 in Macaques,
- Page 17 and 18: Macacine Herpesvirus 1 in Macaques,
- Page 19: Macacine Herpesvirus 1 in Macaques,
- Page 23: Malaria among Young Infants, Africa
- Page 26 and 27: RESEARCHFigure 3. Dynamics of 19-kD
- Page 30 and 31: RESEARCHFigure 2. A) Acoustic trace
- Page 32 and 33: RESEARCHof malaria-infected mosquit
- Page 34 and 35: Lack of Transmission amongClose Con
- Page 36 and 37: RESEARCH(IFA) and microneutralizati
- Page 38 and 39: RESEARCHoropharyngeal, and serum sa
- Page 40 and 41: RESEARCH6. Assiri A, McGeer A, Perl
- Page 42 and 43: RESEARCHadvanced genomic sequencing
- Page 44 and 45: RESEARCHTable 2. Next-generation se
- Page 46 and 47: RESEARCHTable 3. Mutation analysis
- Page 48 and 49: RESEARCHReferences1. Baize S, Panne
- Page 50 and 51: Parechovirus Genotype 3 Outbreakamo
- Page 52 and 53: RESEARCHFigure 1. Venn diagramshowi
- Page 54 and 55: RESEARCHTable 2. HPeV testing of sp
- Page 56 and 57: RESEARCHFigure 5. Distribution of h
- Page 58 and 59: RESEARCHReferences1. Selvarangan R,
- Page 60 and 61: RESEARCHthe left lobe was sampled b
- Page 62 and 63: RESEARCHTable 2. Middle East respir
- Page 64 and 65: RESEARCHseroprevalence in domestic
- Page 66 and 67: RESEARCHmeasure their current surve
- Page 68 and 69: RESEARCHTable 2. States with labora
- Page 70 and 71: RESEARCHFigure 2. Comparison of sur
- Page 72 and 73: RESEARCH9. Centers for Disease Cont
- Page 74 and 75: RESEARCHthe analyses. Cases in pers
- Page 76 and 77: RESEARCHTable 3. Sampling results (
- Page 78 and 79:
RESEARCHpresence of Legionella spp.
- Page 80 and 81:
Seroprevalence for Hepatitis Eand O
- Page 82 and 83:
RESEARCHTable 1. Description of stu
- Page 84 and 85:
RESEARCHTable 3. Crude and adjusted
- Page 86 and 87:
RESEARCHrates by gender or HIV stat
- Page 88 and 89:
RESEARCH25. Taha TE, Kumwenda N, Ka
- Page 90 and 91:
POLICY REVIEWDutch Consensus Guidel
- Page 92 and 93:
POLICY REVIEWTable 3. Comparison of
- Page 94 and 95:
POLICY REVIEW6. Botelho-Nevers E, F
- Page 96 and 97:
DISPATCHESFigure 1. Phylogenetic tr
- Page 98 and 99:
DISPATCHESSevere Pediatric Adenovir
- Page 100 and 101:
DISPATCHESTable 1. Demographics and
- Page 102 and 103:
DISPATCHES13. Kim YJ, Hong JY, Lee
- Page 104 and 105:
DISPATCHESTable. Alignment of resid
- Page 106 and 107:
DISPATCHESFigure 2. Interaction of
- Page 108 and 109:
DISPATCHESSchmallenberg Virus Recur
- Page 110 and 111:
DISPATCHESFigure 2. Detection of Sc
- Page 112 and 113:
DISPATCHESFigure 1. Histopathologic
- Page 114:
DISPATCHESFigure 2. Detection of fo
- Page 117 and 118:
Influenza Virus Strains in the Amer
- Page 119 and 120:
Novel Arenavirus Isolates from Nama
- Page 121 and 122:
Novel Arenaviruses, Southern Africa
- Page 123 and 124:
Readability of Ebola Informationon
- Page 125 and 126:
Readability of Ebola Information on
- Page 127 and 128:
Patients under investigation for ME
- Page 129 and 130:
Patients under investigation for ME
- Page 131 and 132:
Wildlife Reservoir for Hepatitis E
- Page 133 and 134:
Asymptomatic Malaria and Other Infe
- Page 135 and 136:
Asymptomatic Malaria in Children fr
- Page 137 and 138:
Bufavirus in Wild Shrews and Nonhum
- Page 139 and 140:
Bufavirus in Wild Shrews and Nonhum
- Page 141 and 142:
Range Expansion for Rat Lungworm in
- Page 143 and 144:
Slow Clearance of Plasmodium falcip
- Page 145 and 146:
Slow Clearance of Plasmodium falcip
- Page 147 and 148:
Gastroenteritis Caused by Norovirus
- Page 149 and 150:
Ebola Virus Stability on Surfaces a
- Page 151 and 152:
Ebola Virus Stability on Surfaces a
- Page 153 and 154:
Outbreak of Ciprofloxacin-Resistant
- Page 155 and 156:
Outbreak of S. sonnei, South KoreaT
- Page 157 and 158:
Rapidly Expanding Range of Highly P
- Page 159 and 160:
Cluster of Ebola Virus Disease, Bon
- Page 161 and 162:
Cluster of Ebola Virus Disease, Lib
- Page 163 and 164:
ANOTHER DIMENSIONThe Past Is Never
- Page 165 and 166:
Measles Epidemic, Boston, Massachus
- Page 167 and 168:
LETTERSInfluenza A(H5N6)Virus Reass
- Page 169 and 170:
LETTERSsystem (8 kb-span paired-end
- Page 171 and 172:
LETTERS3. Van Hong N, Amambua-Ngwa
- Page 173 and 174:
LETTERSTable. Prevalence of Bartone
- Page 175 and 176:
LETTERSavian influenza A(H5N1) viru
- Page 177 and 178:
LETTERSprovinces and a total of 200
- Page 179 and 180:
LETTERS7. Manian FA. Bloodstream in
- Page 181 and 182:
LETTERSforward projections. N Engl
- Page 183 and 184:
LETTERS3. Guindon S, Gascuel OA. Si
- Page 185 and 186:
BOOKS AND MEDIAin the port cities o
- Page 187 and 188:
ABOUT THE COVERNorth was not intere
- Page 189 and 190:
Earning CME CreditTo obtain credit,
- Page 191:
Emerging Infectious Diseases is a p