research activities in 2007 - CSEM
research activities in 2007 - CSEM
research activities in 2007 - CSEM
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Composite Materials for Bone Implants<br />
M. Giazzon, M. Liley, G. Weder<br />
<strong>CSEM</strong> is develop<strong>in</strong>g methods to nanostructure (‘texture’) composite materials for use <strong>in</strong> orthopaedic implants. Photolithography and bead<br />
lithography methods are used to create master templates that are then replicated <strong>in</strong> a res<strong>in</strong> matrix. The structures will be tested for their effect on<br />
bone cells <strong>in</strong> vitro.<br />
The use of orthopaedic surgery to replace jo<strong>in</strong>ts and repair<br />
bone defects is <strong>in</strong>creas<strong>in</strong>g rapidly. Due to a more active ag<strong>in</strong>g<br />
population, the demands made on the materials used <strong>in</strong> these<br />
operations are also <strong>in</strong>creas<strong>in</strong>g: improved robustness, longer<br />
lifetimes and easier surgical procedures are expected for hip<br />
implants and other jo<strong>in</strong>t replacements.<br />
Metals have been used with enormous success <strong>in</strong> orthopaedic<br />
surgery, but there are still some problems associated with<br />
their use. While issues such as weight and thermal<br />
conductivity can be important for specific applications such as<br />
cranial repair, one major issue of almost universal importance<br />
is that of Young’s modulus. The high stiffness of metallic<br />
implants results <strong>in</strong> a mismatch <strong>in</strong> its mechanical properties<br />
and surround<strong>in</strong>g bone. This <strong>in</strong> turn leads to “stress shield<strong>in</strong>g”:<br />
loss of bone mass and weaken<strong>in</strong>g of the surround<strong>in</strong>g bone<br />
that may lead to implant failure. In this context, the repair of<br />
osteoporotic bone rema<strong>in</strong>s a major challenge.<br />
As a partner <strong>in</strong> the EU project Newbone, <strong>CSEM</strong> is work<strong>in</strong>g to<br />
develop composite materials that can be used <strong>in</strong> orthopaedic<br />
surgery. Glass-fibre re<strong>in</strong>forced composites (FRCs) based on<br />
polymeric materials currently used <strong>in</strong> dentistry are be<strong>in</strong>g<br />
tested and optimised for applications <strong>in</strong> bone repair. <strong>CSEM</strong>’s<br />
contribution is to test the effect of surface coat<strong>in</strong>gs and<br />
modification, with the goal of develop<strong>in</strong>g surface micro- and<br />
nanostructures that enhance cell growth, cell adhesion and<br />
the <strong>in</strong>tegration of the implant <strong>in</strong>to the surround<strong>in</strong>g bone.<br />
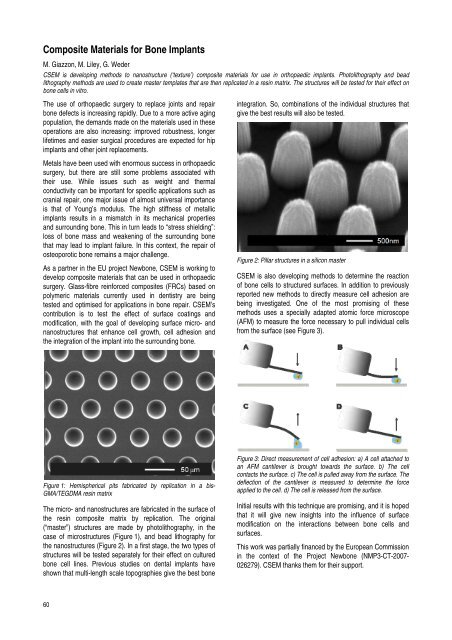
Figure 1: Hemispherical pits fabricated by replication <strong>in</strong> a bis-<br />
GMA/TEGDMA res<strong>in</strong> matrix<br />
The micro- and nanostructures are fabricated <strong>in</strong> the surface of<br />
the res<strong>in</strong> composite matrix by replication. The orig<strong>in</strong>al<br />
(“master”) structures are made by photolithography, <strong>in</strong> the<br />
case of microstructures (Figure 1), and bead lithography for<br />
the nanostructures (Figure 2). In a first stage, the two types of<br />
structures will be tested separately for their effect on cultured<br />
bone cell l<strong>in</strong>es. Previous studies on dental implants have<br />
shown that multi-length scale topographies give the best bone<br />
60<br />
<strong>in</strong>tegration. So, comb<strong>in</strong>ations of the <strong>in</strong>dividual structures that<br />
give the best results will also be tested.<br />
Figure 2: Pillar structures <strong>in</strong> a silicon master<br />
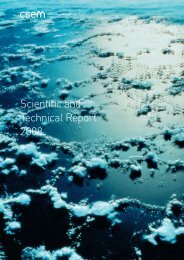
<strong>CSEM</strong> is also develop<strong>in</strong>g methods to determ<strong>in</strong>e the reaction<br />
of bone cells to structured surfaces. In addition to previously<br />
reported new methods to directly measure cell adhesion are<br />
be<strong>in</strong>g <strong>in</strong>vestigated. One of the most promis<strong>in</strong>g of these<br />
methods uses a specially adapted atomic force microscope<br />
(AFM) to measure the force necessary to pull <strong>in</strong>dividual cells<br />
from the surface (see Figure 3).<br />
Figure 3: Direct measurement of cell adhesion: a) A cell attached to<br />
an AFM cantilever is brought towards the surface. b) The cell<br />
contacts the surface. c) The cell is pulled away from the surface. The<br />
deflection of the cantilever is measured to determ<strong>in</strong>e the force<br />
applied to the cell. d) The cell is released from the surface.<br />
Initial results with this technique are promis<strong>in</strong>g, and it is hoped<br />
that it will give new <strong>in</strong>sights <strong>in</strong>to the <strong>in</strong>fluence of surface<br />
modification on the <strong>in</strong>teractions between bone cells and<br />
surfaces.<br />
This work was partially f<strong>in</strong>anced by the European Commission<br />
<strong>in</strong> the context of the Project Newbone (NMP3-CT-<strong>2007</strong>-<br />
026279). <strong>CSEM</strong> thanks them for their support.