9%20ECOGRAFIA%20ABDOMINAL%20COMO%20CUANDO%20DONDE
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
186<br />
ABDOMINAL ULTRASOUND<br />
A<br />
B<br />
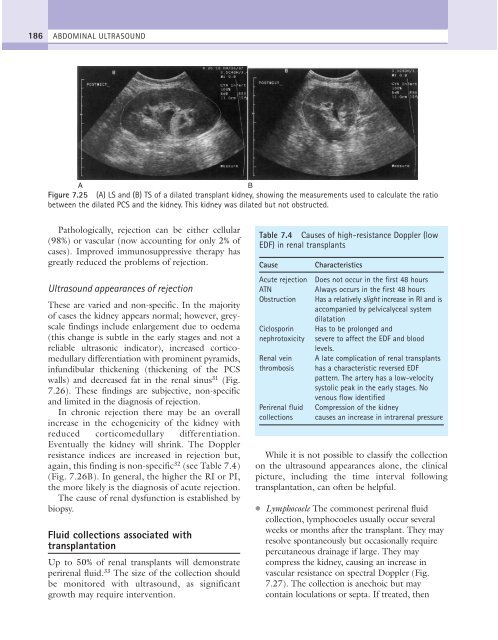
Figure 7.25 (A) LS and (B) TS of a dilated transplant kidney, showing the measurements used to calculate the ratio<br />
between the dilated PCS and the kidney. This kidney was dilated but not obstructed.<br />
Pathologically, rejection can be either cellular<br />
(98%) or vascular (now accounting for only 2% of<br />
cases). Improved immunosuppressive therapy has<br />
greatly reduced the problems of rejection.<br />
Ultrasound appearances of rejection<br />
These are varied and non-specific. In the majority<br />
of cases the kidney appears normal; however, greyscale<br />
findings include enlargement due to oedema<br />
(this change is subtle in the early stages and not a<br />
reliable ultrasonic indicator), increased corticomedullary<br />
differentiation with prominent pyramids,<br />
infundibular thickening (thickening of the PCS<br />
walls) and decreased fat in the renal sinus 31 (Fig.<br />
7.26). These findings are subjective, non-specific<br />
and limited in the diagnosis of rejection.<br />
In chronic rejection there may be an overall<br />
increase in the echogenicity of the kidney with<br />
reduced corticomedullary differentiation.<br />
Eventually the kidney will shrink. The Doppler<br />
resistance indices are increased in rejection but,<br />
again, this finding is non-specific 32 (see Table 7.4)<br />
(Fig. 7.26B). In general, the higher the RI or PI,<br />
the more likely is the diagnosis of acute rejection.<br />
The cause of renal dysfunction is established by<br />
biopsy.<br />
Fluid collections associated with<br />
transplantation<br />
Up to 50% of renal transplants will demonstrate<br />
perirenal fluid. 33 The size of the collection should<br />
be monitored with ultrasound, as significant<br />
growth may require intervention.<br />
Table 7.4 Causes of high-resistance Doppler (low<br />
EDF) in renal transplants<br />
Cause Characteristics<br />
Acute rejection Does not occur in the first 48 hours<br />
ATN<br />
Always occurs in the first 48 hours<br />
Obstruction Has a relatively slight increase in RI and is<br />
accompanied by pelvicalyceal system<br />
dilatation<br />
Ciclosporin Has to be prolonged and<br />
nephrotoxicity severe to affect the EDF and blood<br />
levels.<br />
Renal vein A late complication of renal transplants<br />
thrombosis has a characteristic reversed EDF<br />
pattern. The artery has a low-velocity<br />
systolic peak in the early stages. No<br />
venous flow identified<br />
Perirenal fluid Compression of the kidney<br />
collections causes an increase in intrarenal pressure<br />
While it is not possible to classify the collection<br />
on the ultrasound appearances alone, the clinical<br />
picture, including the time interval following<br />
transplantation, can often be helpful.<br />
●<br />
Lymphocoele The commonest perirenal fluid<br />
collection, lymphocoeles usually occur several<br />
weeks or months after the transplant. They may<br />
resolve spontaneously but occasionally require<br />
percutaneous drainage if large. They may<br />
compress the kidney, causing an increase in<br />
vascular resistance on spectral Doppler (Fig.<br />
7.27). The collection is anechoic but may<br />
contain loculations or septa. If treated, then