Research Group Heussler (Malaria I) - Bernhard-Nocht-Institut für ...
Research Group Heussler (Malaria I) - Bernhard-Nocht-Institut für ...
Research Group Heussler (Malaria I) - Bernhard-Nocht-Institut für ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
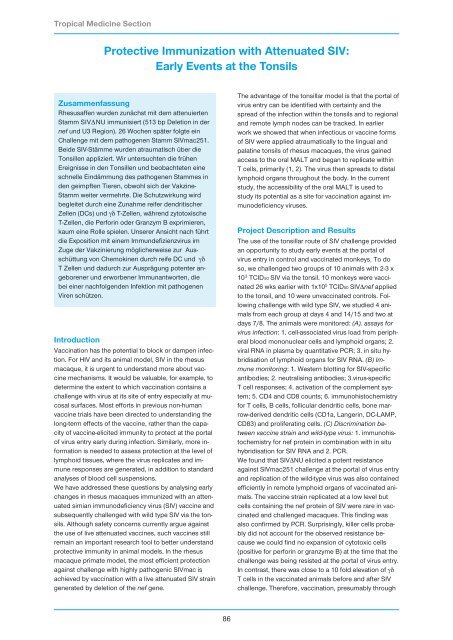
Tropical Medicine Section<br />
Protective Immunization with Attenuated SIV:<br />
Early Events at the Tonsils<br />
Zusammenfassung<br />
Rhesusaffen wurden zunächst mit dem attenuierten<br />
Stamm SIV∆NU immunisiert (513 bp Deletion in der<br />
nef und U3 Region). 26 Wochen später folgte ein<br />
Challenge mit dem pathogenen Stamm SIVmac251.<br />
Beide SIV-Stämme wurden atraumatisch über die<br />
Tonsillen appliziert. Wir untersuchten die frühen<br />
Ereignisse in den Tonsillen und beobachteten eine<br />
schnelle Eindämmung des pathogenen Stammes in<br />
den geimpften Tieren, obwohl sich der Vakzine-<br />
Stamm weiter vermehrte. Die Schutzwirkung wird<br />
begleitet durch eine Zunahme reifer dendritischer<br />
Zellen (DCs) und γδ T-Zellen, während zytotoxische<br />
T-Zellen, die Perforin oder Granzym B exprimieren,<br />
kaum eine Rolle spielen. Unserer Ansicht nach führt<br />
die Exposition mit einem Immundefizienzvirus im<br />
Zuge der Vakzinierung möglicherweise zur Ausschüttung<br />
von Chemokinen durch reife DC und γδ<br />
T Zellen und dadurch zur Ausprägung potenter angeborener<br />
und erworbener Immunantworten, die<br />
bei einer nachfolgenden Infektion mit pathogenen<br />
Viren schützen.<br />
Introduction<br />
Vaccination has the potential to block or dampen infection.<br />
For HIV and its animal model, SIV in the rhesus<br />
macaque, it is urgent to understand more about vaccine<br />
mechanisms. It would be valuable, for example, to<br />
determine the extent to which vaccination contains a<br />
challenge with virus at its site of entry especially at mucosal<br />
surfaces. Most efforts in previous non-human<br />
vaccine trials have been directed to understanding the<br />
long-term effects of the vaccine, rather than the capacity<br />
of vaccine-elicited immunity to protect at the portal<br />
of virus entry early during infection. Similarly, more information<br />
is needed to assess protection at the level of<br />
lymphoid tissues, where the virus replicates and immune<br />
responses are generated, in addition to standard<br />
analyses of blood cell suspensions.<br />
We have addressed these questions by analysing early<br />
changes in rhesus macaques immunized with an attenuated<br />
simian immunodeficiency virus (SIV) vaccine and<br />
subsequently challenged with wild type SIV via the tonsils.<br />
Although safety concerns currently argue against<br />
the use of live attenuated vaccines, such vaccines still<br />
remain an important research tool to better understand<br />
protective immunity in animal models. In the rhesus<br />
macaque primate model, the most efficient protection<br />
against challenge with highly pathogenic SIVmac is<br />
achieved by vaccination with a live attenuated SIV strain<br />
generated by deletion of the nef gene.<br />
86<br />
The advantage of the tonsillar model is that the portal of<br />
virus entry can be identified with certainty and the<br />
spread of the infection within the tonsils and to regional<br />
and remote lymph nodes can be tracked. In earlier<br />
work we showed that when infectious or vaccine forms<br />
of SIV were applied atraumatically to the lingual and<br />
palatine tonsils of rhesus macaques, the virus gained<br />
access to the oral MALT and began to replicate within<br />
T cells, primarily (1, 2). The virus then spreads to distal<br />
lymphoid organs throughout the body. In the current<br />
study, the accessibility of the oral MALT is used to<br />
study its potential as a site for vaccination against immunodeficiency<br />
viruses.<br />
Project Description and Results<br />
The use of the tonsillar route of SIV challenge provided<br />
an opportunity to study early events at the portal of<br />
virus entry in control and vaccinated monkeys. To do<br />
so, we challenged two groups of 10 animals with 2-3 x<br />
10 3 TCID50 SIV via the tonsil. 10 monkeys were vaccinated<br />
26 wks earlier with 1x10 5 TCID50 SIV∆nef applied<br />
to the tonsil, and 10 were unvaccinated controls. Following<br />
challenge with wild type SIV, we studied 4 animals<br />
from each group at days 4 and 14/15 and two at<br />
days 7/8. The animals were monitored: (A). assays for<br />
virus infection: 1. cell-associated virus load from peripheral<br />
blood mononuclear cells and lymphoid organs; 2.<br />
viral RNA in plasma by quantitative PCR; 3. in situ hybridisation<br />
of lymphoid organs for SIV RNA. (B) Immune<br />
monitoring: 1. Western blotting for SIV-specific<br />
antibodies; 2. neutralising antibodies; 3.virus-specific<br />
T cell responses; 4. activation of the complement system;<br />
5. CD4 and CD8 counts; 6. immunohistochemistry<br />
for T cells, B cells, follicular dendritic cells, bone marrow-derived<br />
dendritic cells (CD1a, Langerin, DC-LAMP,<br />
CD83) and proliferating cells. (C) Discrimination between<br />
vaccine strain and wild-type virus: 1. immunohistochemistry<br />
for nef protein in combination with in situ<br />
hybridisation for SIV RNA and 2. PCR.<br />
We found that SIV∆NU elicited a potent resistance<br />
against SIVmac251 challenge at the portal of virus entry<br />
and replication of the wild-type virus was also contained<br />
efficiently in remote lymphoid organs of vaccinated animals.<br />
The vaccine strain replicated at a low level but<br />
cells containing the nef protein of SIV were rare in vaccinated<br />
and challenged macaques. This finding was<br />
also confirmed by PCR. Surprisingly, killer cells probably<br />
did not account for the observed resistance because<br />
we could find no expansion of cytotoxic cells<br />
(positive for perforin or granzyme B) at the time that the<br />
challenge was being resisted at the portal of virus entry.<br />
In contrast, there was close to a 10 fold elevation of γδ<br />
T cells in the vaccinated animals before and after SIV<br />
challenge. Therefore, vaccination, presumably through