- Page 1 and 2:
The Honorable Kathleen Sebelius Sec
- Page 3 and 4:
promote the integration and full in
- Page 5 and 6:
The National Pediatric Acquired Bra
- Page 7:
Phase Three consisted of having the
- Page 10 and 11:
the fact that their brains are stil
- Page 12 and 13: methods developed by the SJBP to sh
- Page 14 and 15: Two-Year Milestones Quarter 1: •
- Page 16 and 17: Figure 2: CDC figures for death and
- Page 18 and 19: PA/TBI and their families, delivere
- Page 20 and 21: appropriately in the care of the ch
- Page 22 and 23: CHAPTER 2: The TBI Model System and
- Page 24 and 25: 2. States need to “buy” into id
- Page 26 and 27: implications of shaking a baby; and
- Page 28 and 29: service was developed for children
- Page 30 and 31: a. There is a lack of evidence for
- Page 32 and 33: 8. In addition, ongoing education a
- Page 34 and 35: While there are often significant i
- Page 36 and 37: are largely unknown. In particular,
- Page 38 and 39: Family Perspective: Without early i
- Page 40 and 41: 4. Improve the specific identificat
- Page 42 and 43: unemployment, public-assisted housi
- Page 44 and 45: REFERRAL FROM ACUTE CARE, REHABILIT
- Page 46 and 47: understanding determinants of long-
- Page 48 and 49: Research - Increase capacity of loc
- Page 50 and 51: Alternatively, indirect effects on
- Page 52 and 53: Specific questions regarding tracki
- Page 54 and 55: CHAPTER 7: Categories of Care: Tran
- Page 56 and 57: care of syndromes associated with a
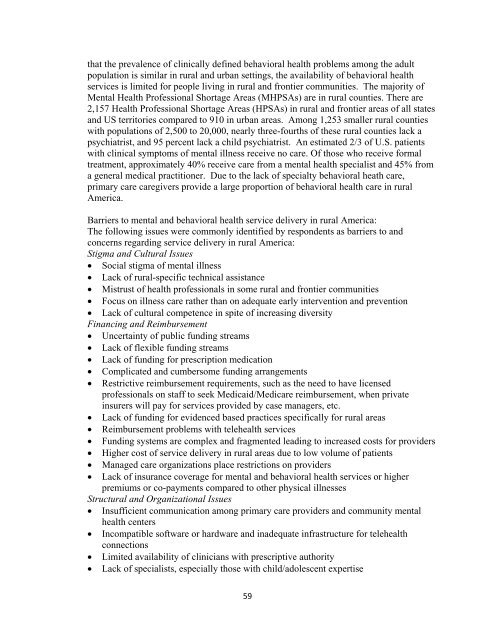
- Page 58 and 59: Social Opportunities The services a
- Page 60 and 61: Finally, a third area of problem af
- Page 64 and 65: • Lack of public transportation
- Page 66 and 67: • Provide consequences for wastin
- Page 68 and 69: Rural / Tele-health issues during A
- Page 70 and 71: educated and thus are less aware of
- Page 72 and 73: Chapter 9: Category of Care: The Vi
- Page 74 and 75: "To improve the quality of our heal
- Page 76 and 77: Registry technology has been used a
- Page 78 and 79: CHAPTER 10: Organizational Structur
- Page 80 and 81: Northeast Region: New York Mid-Atla
- Page 82 and 83: State IT Manager: primary responsib
- Page 84 and 85: translational data for their Catego
- Page 86 and 87: CHAPTER 11: Financing the PABI Plan
- Page 88 and 89: projects, a smaller state will have
- Page 90 and 91: Summary of PABI Grant Proposal cont
- Page 92 and 93: Sarah Jane Brain Family State Lead
- Page 94 and 95: The University of Alabama at Birmin
- Page 96 and 97: h Principal Investigator/Program Di
- Page 98 and 99: Sarah Jane Brain Family State Lead
- Page 100 and 101: The Children's Hospital at Providen
- Page 102 and 103: Sarah Jane Brain Family State Lead
- Page 104 and 105: Barrow Neurological Institute / St.
- Page 106 and 107: Employment Education Postgraduate T
- Page 108 and 109: Certifications Neuroscience Grand R
- Page 110 and 111: Sarah Jane Brain Family State Lead
- Page 112 and 113:
UAMS/Arkansas Children's Hospital R
- Page 114 and 115:
Program Director/Principal Investig
- Page 116 and 117:
C. Research Support Ongoing Researc
- Page 118 and 119:
Sarah Jane Brain Family State Lead
- Page 120 and 121:
Mattel Children's Hospital UCLA Pro
- Page 122 and 123:
BIOGRAPHICAL SKETCH Provide the fol
- Page 124 and 125:
17. Madikians A and Giza CC. A Clin
- Page 126 and 127:
Sarah Jane Brain Family State Lead
- Page 128 and 129:
The Children's Hospital Profile con
- Page 130 and 131:
CURRICULUM VITAE JEANNE E. DISE, Ph
- Page 132 and 133:
Curriculum Vitae Jeanne E. Dise Pag
- Page 134 and 135:
Curriculum Vitae Jeanne E. Dise Pag
- Page 136 and 137:
Curriculum Vitae Jeanne E. Dise Pag
- Page 138 and 139:
Curriculum Vitae Jeanne E. Dise Pag
- Page 140 and 141:
Curriculum Vitae Jeanne E. Dise Pag
- Page 142 and 143:
Curriculum Vitae Jeanne E. Dise Pag
- Page 144 and 145:
Curriculum Vitae Jeanne E. Dise Pag
- Page 146 and 147:
Curriculum Vitae Jeanne E. Dise Pag
- Page 148 and 149:
Curriculum Vitae Jeanne E. Dise Pag
- Page 150 and 151:
Curriculum Vitae Jeanne E. Dise Pag
- Page 152 and 153:
Yale‐New Haven Children's Hospita
- Page 154 and 155:
Yale‐New Haven Children's Hospita
- Page 156 and 157:
2001 - Associate Professor, Sect of
- Page 158 and 159:
Major goal: to provide education in
- Page 160 and 161:
Sarah Jane Brain Family State Lead
- Page 162 and 163:
Nemours / Alfred I. duPont Hospital
- Page 164 and 165:
First Name: Michael MI: A Last Name
- Page 166 and 167:
Sarah Jane Brain Family State Lead
- Page 168 and 169:
Children's National Medical Center
- Page 170 and 171:
Program Director/Principal Investig
- Page 172 and 173:
Program Director/Principal Investig
- Page 174 and 175:
Sarah Jane Brain Family State Lead
- Page 176 and 177:
University of Miami Miller School o
- Page 178 and 179:
FF Principal Investigator/Program D
- Page 180 and 181:
FF Principal Investigator/Program D
- Page 182 and 183:
FF Principal Investigator/Program D
- Page 184 and 185:
Huang TT, He D, Kleiner G, Kuluz J.
- Page 186 and 187:
Children's Healthcare of Atlanta Pr
- Page 188 and 189:
Children's Healthcare of Atlanta Pr
- Page 190 and 191:
Principal Investigator: Haarbauer-K
- Page 192 and 193:
Sarah Jane Brain Family State Lead
- Page 194 and 195:
Center on Disability Studies at The
- Page 196 and 197:
Jean L. Johnson, DrPH April 19, 200
- Page 198 and 199:
Jeffrey K. Okamoto M.D. Curriculum
- Page 200 and 201:
Sarah Jane Brain Family State Lead
- Page 202 and 203:
Idaho State University / Institute
- Page 204 and 205:
NAME RUSSELL C. SPEARMAN BIOGRAPHIC
- Page 206 and 207:
Spearman, Russell, C Spearman, R.C.
- Page 208 and 209:
RESEARCH FUNDING Current Support: I
- Page 210 and 211:
University of Illinois Chicago Prof
- Page 212 and 213:
University of Illinois Chicago Prof
- Page 214 and 215:
1997 Margaret Faust Thesis Award, S
- Page 216 and 217:
Sarah Jane Brain Family State Lead
- Page 218 and 219:
James Whitcomb Riley Hospital for C
- Page 220 and 221:
PROGRAM DIRECTOR: Jodi L. Smith, Ph
- Page 222 and 223:
American Association of Anatomists
- Page 224 and 225:
IU Faculty Steering Committee ‐ 7
- Page 226 and 227:
Sarah Jane Brain Family State Lead
- Page 228 and 229:
University of Iowa Children's Hospi
- Page 230 and 231:
NAME Lindgren, Scott D. eRA COMMONS
- Page 232 and 233:
Arroyos-Jurado, E., Paulsen, J.S.,
- Page 234 and 235:
Center for Child Health and Develop
- Page 236 and 237:
Center for Child Health and Develop
- Page 238 and 239:
Tyler 2 Glang, A., Dise-Lewis, J.,
- Page 240 and 241:
Tyler 4 DePompei, R., Glang, A., &
- Page 242 and 243:
University of Kentucky Hospital Pro
- Page 244 and 245:
University of Kentucky Hospital Pro
- Page 246 and 247:
Joseph A. Iocono, M.D. Curriculum V
- Page 248 and 249:
Joseph A. Iocono, M.D. Curriculum V
- Page 250 and 251:
Joseph A. Iocono, M.D. Curriculum V
- Page 252 and 253:
Joseph A. Iocono, M.D. Curriculum V
- Page 254 and 255:
Joseph A. Iocono, M.D. Curriculum V
- Page 256 and 257:
Joseph A. Iocono, M.D Curriculum Vi
- Page 258 and 259:
Joseph A. Iocono, M.D. Curriculum V
- Page 260 and 261:
Joseph A. Iocono, M.D Curriculum Vi
- Page 262 and 263:
Joseph A. Iocono, M.D Curriculum Vi
- Page 264 and 265:
Joseph A. Iocono, M.D Curriculum Vi
- Page 266 and 267:
Joseph A. Iocono, M.D Curriculum Vi
- Page 268 and 269:
Sarah Jane Brain Family State Lead
- Page 270 and 271:
Louisiana Health Care Quality Forum
- Page 272 and 273:
Shannon Robshaw, MSW is the Executi
- Page 274 and 275:
Maine Institute of Human Genetics a
- Page 276 and 277:
Maine Institute of Human Genetics a
- Page 278 and 279:
Principal Investigator/Program Dire
- Page 280 and 281:
Principal Investigator/Program Dire
- Page 282 and 283:
Kennedy Krieger Institute Profile c
- Page 284 and 285:
Kennedy Krieger Institute Profile c
- Page 286 and 287:
Principal Investigator/Program Dire
- Page 288 and 289:
Principal Investigator/Program Dire
- Page 290 and 291:
Program Director/Principal Investig
- Page 292 and 293:
Sarah Jane Brain Family State Lead
- Page 294 and 295:
Children's Hospital of Boston and H
- Page 296 and 297:
Date Updated: November 5, 2008 CURR
- Page 298 and 299:
2001- Member, Advisory Committee Ha
- Page 300 and 301:
underway to best direct prevention
- Page 302 and 303:
2. Mooney DP, Lewis JE, Connors RH,
- Page 304 and 305:
40. Waltzman M, Baskin M, Wypij D,
- Page 306 and 307:
19. Downard C and Mooney DP. Pediat
- Page 308 and 309:
47. Kangas KK, Lee LK, Forbes P, Os
- Page 310 and 311:
29. Kansas Trauma Conference, Wichi
- Page 312 and 313:
Date Prepared: January 5, 2009 Name
- Page 314 and 315:
Regional 2006- Vice President of Ma
- Page 316 and 317:
Honors and Prizes Year Name of Hono
- Page 318 and 319:
2000 Pediatric Spine Injuries Singl
- Page 320 and 321:
2006 Infant Skull Deformities Pedia
- Page 322 and 323:
2002 Management of Sports-related C
- Page 324 and 325:
Clinical Innovations I have been ab
- Page 326 and 327:
10. Dunn IF, Proctor MR, Day AL. Lu
- Page 328 and 329:
Trauma Surgery, Neurology, Neuropsy
- Page 330 and 331:
Michigan Public Health Institute an
- Page 332 and 333:
Michigan Public Health Institute an
- Page 334 and 335:
Vonderheid, S.C., Pohl, J. M., Tann
- Page 336 and 337:
Mayo Clinic Profile continued Title
- Page 338 and 339:
Mayo Clinic Profile continued Title
- Page 340 and 341:
LICENSURE Minnesota HONORS/AWARDS S
- Page 342 and 343:
Spina Bifida in Adulthood Physical
- Page 344 and 345:
Sherilyn W. Driscoll, MD Page 6 of
- Page 346 and 347:
-Implementation of new pediatric wh
- Page 348 and 349:
BIBLIOGRAPHY Peer-reviewed Articles
- Page 350 and 351:
Program Director/Principal Investig
- Page 352 and 353:
Sarah Jane Brain Family State Lead
- Page 354 and 355:
Children's Rehabilitation Services
- Page 356 and 357:
Curriculum Vitae Shannon Janine Smi
- Page 358 and 359:
Shannon Janine Smith, MD Page 2 Hon
- Page 360 and 361:
Center, Pediatric Grand Rounds Shan
- Page 362 and 363:
Saint Louis Children's Hospital Pro
- Page 364 and 365:
Saint Louis Children's Hospital Pro
- Page 366 and 367:
Principal Investigator/Program Dire
- Page 368 and 369:
Completed Research Support Principa
- Page 370 and 371:
Montana State University Billings /
- Page 372 and 373:
Montana State University Billings /
- Page 374 and 375:
• Region IV Paraeducator Summer I
- Page 376 and 377:
Madonna Rehabilitation Hospital Pro
- Page 378 and 379:
Madonna Rehabilitation Hospital Pro
- Page 380 and 381:
Staff Occupational Therapist: 1997-
- Page 382 and 383:
Sunrise Children's Hospital Profile
- Page 384 and 385:
Sunrise Children's Hospital Profile
- Page 386 and 387:
Sarah Jane Brain Family State Lead
- Page 388 and 389:
Dartmouth Medical School Profile co
- Page 390 and 391:
BIOGRAPHICAL SKETCH NAME POSITION T
- Page 392 and 393:
Sarah Jane Brain Family State Lead
- Page 394 and 395:
Brain Injury Association of New Jer
- Page 396 and 397:
Biographical Sketch Barbara Geiger-
- Page 398 and 399:
Sarah Jane Brain Family State Lead
- Page 400 and 401:
University of New Mexico School of
- Page 402 and 403:
Sarah Jane Brain Family State Lead
- Page 404 and 405:
Mount Sinai Medical Center Profile
- Page 410 and 411:
Sarah Jane Brain Family State Lead
- Page 412 and 413:
The Clinical Center for the Study o
- Page 414 and 415:
NAME Stephen R. Hooper eRA COMMONS
- Page 416 and 417:
Hooper, S.R., Hatton, D., Schaaf, J
- Page 418 and 419:
Sarah Jane Brain Family State Lead
- Page 420 and 421:
Still pending Profile continued Tit
- Page 422 and 423:
Sarah Jane Brain Family State Lead
- Page 424 and 425:
Cincinnati Children's Hospital Medi
- Page 426 and 427:
Principal Investigator/Program Dire
- Page 428 and 429:
Principal Investigator/Program Dire
- Page 430 and 431:
Sarah Jane Brain Family State Lead
- Page 432 and 433:
Oklahoma State University / Center
- Page 434 and 435:
CURRICULUM VITAE NAME Stanley E. Gr
- Page 436 and 437:
Courtesy Staff, 1990-1998 Leave of
- Page 438 and 439:
OSU-CHS International Medicine Club
- Page 440 and 441:
ViroPharma Protocol 637-303: Princi
- Page 442 and 443:
Media presentations: Medical Minute
- Page 444 and 445:
Sarah Jane Brain Family State Lead
- Page 446 and 447:
Teaching Research Institute and Wes
- Page 448 and 449:
BIOGRAPHICAL SKETCH NAME POSITION T
- Page 450 and 451:
Voss, J., Stevens, T., Glang, A., &
- Page 452 and 453:
Sarah Jane Brain Family State Lead
- Page 454 and 455:
Children's Hospital of Pittsburgh o
- Page 456 and 457:
BIOGRAPHICAL SKETCH Provide the fol
- Page 458 and 459:
C. Research Support. List selected
- Page 460 and 461:
Puerto Rico Medical Center / Univer
- Page 462 and 463:
Puerto Rico Medical Center / Univer
- Page 464 and 465:
LICENCE TO PRACTICE MEDICINE: (plac
- Page 466 and 467:
REFERENCES Dr. Nathan Rifkinson, UP
- Page 468 and 469:
Hasbro Children's Hospital Child Pr
- Page 470 and 471:
Hasbro Children's Hospital Child Pr
- Page 472 and 473:
1990-1996 Director of Medical Progr
- Page 474 and 475:
infant death and suspected physical
- Page 476 and 477:
Medical University of South Carolin
- Page 478 and 479:
Medical University of South Carolin
- Page 480 and 481:
Principal Investigator/Program Dire
- Page 482 and 483:
Role: PI Principal Investigator/Pro
- Page 484 and 485:
Center for Disabilities / Sanford S
- Page 486 and 487:
Center for Disabilities / Sanford S
- Page 488 and 489:
• February 2004 - May 2005: Indep
- Page 490 and 491:
• September 2008: Presentation at
- Page 492 and 493:
• Coordinator for LEND (The South
- Page 494 and 495:
University of Tennessee Profile con
- Page 496 and 497:
University of Tennessee Profile con
- Page 498 and 499:
4. Johnson, R. K., Hough, M. S., Ki
- Page 500 and 501:
Center for BrainHealth / The Univer
- Page 502 and 503:
Center for BrainHealth / The Univer
- Page 504 and 505:
McCauley, S.R., McDaniel, M.A., Ped
- Page 506 and 507:
Levin, H. S., Mendelsohn, D. B., Li
- Page 508 and 509:
University of Utah Profile continue
- Page 510 and 511:
University of Utah Profile continue
- Page 512 and 513:
5. Statler KD, Jenkins LW, Dixon CE
- Page 514 and 515:
F. Invited Presentations Internatio
- Page 516 and 517:
The Vermont Center for Children, Yo
- Page 518 and 519:
The Vermont Center for Children, Yo
- Page 520 and 521:
2006-Present Chairman of the Child
- Page 522 and 523:
Abdellaoui A, Bartels M, Hudziak JJ
- Page 524 and 525:
UVA Children's Hospital and Kluge's
- Page 526 and 527:
UVA Children's Hospital and Kluge's
- Page 528 and 529:
B. Selected peer-reviewed publicati
- Page 530 and 531:
University of Washington / Harborvi
- Page 532 and 533:
University of Washington / Harborvi
- Page 534 and 535:
Principal Investigator/Program Dire
- Page 536 and 537:
Principal Investigator/Program Dire
- Page 538 and 539:
Principal Investigator/Program Dire
- Page 540 and 541:
West Virginia Brain Injury Associat
- Page 542 and 543:
West Virginia Brain Injury Associat
- Page 544 and 545:
Phone: (304) 345-7757 405 Capitol S
- Page 546 and 547:
Children's Hospital of Wisconsin Pr
- Page 548 and 549:
Children's Hospital of Wisconsin Pr
- Page 550 and 551:
Principal Investigator/Program Dire
- Page 552 and 553:
Sarah Jane Brain Family State Lead
- Page 554 and 555:
Brain Injury Association of Wyoming
- Page 556 and 557:
EDUCATION Dorothy Worrell 2302 Sage
- Page 558 and 559:
of Developmental Disabilities; assi
- Page 560 and 561:
PUBLICATIONS Member of VISIONS Admi
- Page 562 and 563:
Sarah Jane Brain Family State Lead
- Page 564 and 565:
n/a Profile continued Title/Descrip
- Page 566 and 567:
References 1. Adelson, P.D. (2008).
- Page 568 and 569:
30. Centers for Disease Control and
- Page 570 and 571:
62. Haddon, W. (1973). Energy damag
- Page 572 and 573:
96. Perel, P., Yanagawa, T., Bunn,