The Design of Diagnostic Medical Facilities where ... - ResearchGate
The Design of Diagnostic Medical Facilities where ... - ResearchGate
The Design of Diagnostic Medical Facilities where ... - ResearchGate
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
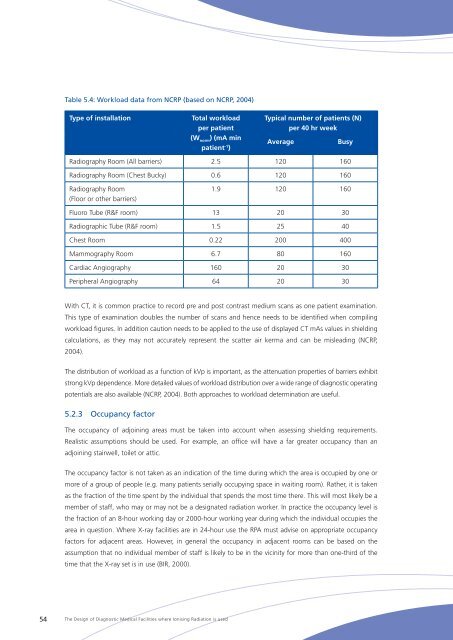
Table 5.4: Workload data from NCRP (based on NCRP, 2004)<br />
Type <strong>of</strong> installation<br />
Total workload<br />
per patient<br />
(W norm<br />
) (mA min<br />
patient -1 )<br />
Typical number <strong>of</strong> patients (N)<br />
per 40 hr week<br />
Average<br />
Busy<br />
Radiography Room (All barriers) 2.5 120 160<br />
Radiography Room (Chest Bucky) 0.6 120 160<br />
Radiography Room<br />
(Floor or other barriers)<br />
1.9 120 160<br />
Fluoro Tube (R&F room) 13 20 30<br />
Radiographic Tube (R&F room) 1.5 25 40<br />
Chest Room 0.22 200 400<br />
Mammography Room 6.7 80 160<br />
Cardiac Angiography 160 20 30<br />
Peripheral Angiography 64 20 30<br />
With CT, it is common practice to record pre and post contrast medium scans as one patient examination.<br />
This type <strong>of</strong> examination doubles the number <strong>of</strong> scans and hence needs to be identified when compiling<br />
workload figures. In addition caution needs to be applied to the use <strong>of</strong> displayed CT mAs values in shielding<br />
calculations, as they may not accurately represent the scatter air kerma and can be misleading (NCRP,<br />
2004).<br />
<strong>The</strong> distribution <strong>of</strong> workload as a function <strong>of</strong> kVp is important, as the attenuation properties <strong>of</strong> barriers exhibit<br />
strong kVp dependence. More detailed values <strong>of</strong> workload distribution over a wide range <strong>of</strong> diagnostic operating<br />
potentials are also available (NCRP, 2004). Both approaches to workload determination are useful.<br />
5.2.3 Occupancy factor<br />
<strong>The</strong> occupancy <strong>of</strong> adjoining areas must be taken into account when assessing shielding requirements.<br />
Realistic assumptions should be used. For example, an <strong>of</strong>fice will have a far greater occupancy than an<br />
adjoining stairwell, toilet or attic.<br />
<strong>The</strong> occupancy factor is not taken as an indication <strong>of</strong> the time during which the area is occupied by one or<br />
more <strong>of</strong> a group <strong>of</strong> people (e.g. many patients serially occupying space in waiting room). Rather, it is taken<br />
as the fraction <strong>of</strong> the time spent by the individual that spends the most time there. This will most likely be a<br />
member <strong>of</strong> staff, who may or may not be a designated radiation worker. In practice the occupancy level is<br />
the fraction <strong>of</strong> an 8-hour working day or 2000-hour working year during which the individual occupies the<br />
area in question. Where X‐ray facilities are in 24-hour use the RPA must advise on appropriate occupancy<br />
factors for adjacent areas. However, in general the occupancy in adjacent rooms can be based on the<br />
assumption that no individual member <strong>of</strong> staff is likely to be in the vicinity for more than one-third <strong>of</strong> the<br />
time that the X‐ray set is in use (BIR, 2000).<br />
54<br />
<strong>The</strong> <strong>Design</strong> <strong>of</strong> <strong>Diagnostic</strong> <strong>Medical</strong> <strong>Facilities</strong> <strong>where</strong> Ionising Radiation is used