Hand hygiene.pdf
Hand hygiene.pdf
Hand hygiene.pdf
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
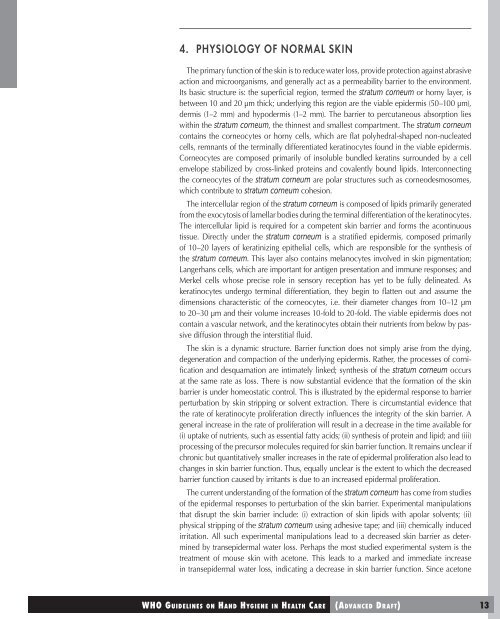
4. PHYSIOLOGY OF NORMAL SKIN<br />
The primary function of the skin is to reduce water loss, provide protection against abrasive<br />
action and microorganisms, and generally act as a permeability barrier to the environment.<br />
Its basic structure is: the superficial region, termed the stratum corneum or horny layer, is<br />
between 10 and 20 μm thick; underlying this region are the viable epidermis (50–100 μm),<br />
dermis (1–2 mm) and hypodermis (1–2 mm). The barrier to percutaneous absorption lies<br />
within the stratum corneum, the thinnest and smallest compartment. The stratum corneum<br />
contains the corneocytes or horny cells, which are flat polyhedral-shaped non-nucleated<br />
cells, remnants of the terminally differentiated keratinocytes found in the viable epidermis.<br />
Corneocytes are composed primarily of insoluble bundled keratins surrounded by a cell<br />
envelope stabilized by cross-linked proteins and covalently bound lipids. Interconnecting<br />
the corneocytes of the stratum corneum are polar structures such as corneodesmosomes,<br />
which contribute to stratum corneum cohesion.<br />
The intercellular region of the stratum corneum is composed of lipids primarily generated<br />
from the exocytosis of lamellar bodies during the terminal differentiation of the keratinocytes.<br />
The intercellular lipid is required for a competent skin barrier and forms the acontinuous<br />
tissue. Directly under the stratum corneum is a stratified epidermis, composed primarily<br />
of 10–20 layers of keratinizing epithelial cells, which are responsible for the synthesis of<br />
the stratum corneum. This layer also contains melanocytes involved in skin pigmentation;<br />
Langerhans cells, which are important for antigen presentation and immune responses; and<br />
Merkel cells whose precise role in sensory reception has yet to be fully delineated. As<br />
keratinocytes undergo terminal differentiation, they begin to flatten out and assume the<br />
dimensions characteristic of the corneocytes, i.e. their diameter changes from 10–12 μm<br />
to 20–30 μm and their volume increases 10-fold to 20-fold. The viable epidermis does not<br />
contain a vascular network, and the keratinocytes obtain their nutrients from below by passive<br />
diffusion through the interstitial fluid.<br />
The skin is a dynamic structure. Barrier function does not simply arise from the dying,<br />
degeneration and compaction of the underlying epidermis. Rather, the processes of cornification<br />
and desquamation are intimately linked; synthesis of the stratum corneum occurs<br />
at the same rate as loss. There is now substantial evidence that the formation of the skin<br />
barrier is under homeostatic control. This is illustrated by the epidermal response to barrier<br />
perturbation by skin stripping or solvent extraction. There is circumstantial evidence that<br />
the rate of keratinocyte proliferation directly influences the integrity of the skin barrier. A<br />
general increase in the rate of proliferation will result in a decrease in the time available for<br />
(i) uptake of nutrients, such as essential fatty acids; (ii) synthesis of protein and lipid; and (iii)<br />
processing of the precursor molecules required for skin barrier function. It remains unclear if<br />
chronic but quantitatively smaller increases in the rate of epidermal proliferation also lead to<br />
changes in skin barrier function. Thus, equally unclear is the extent to which the decreased<br />
barrier function caused by irritants is due to an increased epidermal proliferation.<br />
The current understanding of the formation of the stratum corneum has come from studies<br />
of the epidermal responses to perturbation of the skin barrier. Experimental manipulations<br />
that disrupt the skin barrier include: (i) extraction of skin lipids with apolar solvents; (ii)<br />
physical stripping of the stratum corneum using adhesive tape; and (iii) chemically induced<br />
irritation. All such experimental manipulations lead to a decreased skin barrier as determined<br />
by transepidermal water loss. Perhaps the most studied experimental system is the<br />
treatment of mouse skin with acetone. This leads to a marked and immediate increase<br />
in transepidermal water loss, indicating a decrease in skin barrier function. Since acetone