Docetaxel with prednisone or prednisolone for the treatment of ...
Docetaxel with prednisone or prednisolone for the treatment of ...
Docetaxel with prednisone or prednisolone for the treatment of ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
132<br />
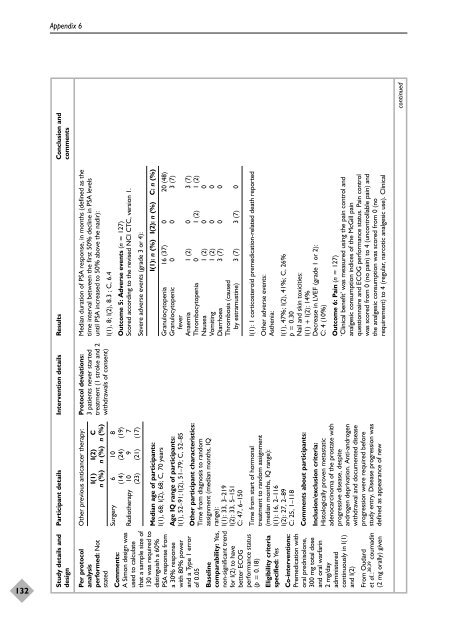
Appendix 6<br />
Study details and Participant details Intervention details Results Conclusion and<br />
design comments<br />
Median duration <strong>of</strong> PSA response, in months (defined as <strong>the</strong><br />
time interval between <strong>the</strong> first 50% decline in PSA levels<br />
until PSA increased to 50% above <strong>the</strong> nadir):<br />
Protocol deviations:<br />
3 patients never started<br />
<strong>treatment</strong> (1 stroke and 2<br />
<strong>with</strong>drawals <strong>of</strong> consent)<br />
O<strong>the</strong>r previous anticancer <strong>the</strong>rapy:<br />
I(1) I(2) C<br />
n (%) n (%) n (%)<br />
Per protocol<br />
analysis<br />
perf<strong>or</strong>med: Not<br />
stated<br />
I(1), 8; I(2), 8.3 ; C, 6.4<br />
Outcome 5: Adverse events (n = 127)<br />
Sc<strong>or</strong>ed acc<strong>or</strong>ding to <strong>the</strong> revised NCI CTC, version 1.<br />
Surgery 6 10 8<br />
(14) (24) (19)<br />
Radio<strong>the</strong>rapy 10 9 7<br />
(23) (21) (17)<br />
Severe adverse events (grade 3 <strong>or</strong> 4):<br />
I(1): n (%) I(2): n (%) C: n (%)<br />
Median age <strong>of</strong> participants:<br />
I(1), 68; I(2), 68; C, 70 years<br />
Granulocytopenia 16 (37) 0 20 (48)<br />
Granulocytopenic 0 0 3 (7)<br />
fever<br />
Anaemia 1 (2) 0 3 (7)<br />
Thrombocytopenia 0 1 (2) 1 (2)<br />
Nausea 1 (2) 0 0<br />
Vomiting 1 (2) 0 0<br />
Diarrhoea 3 (7) 0 0<br />
Thrombosis (caused<br />
by estramustine) 3 (7) 3 (7) 0<br />
Age IQ range <strong>of</strong> participants:<br />
I(1), 52–91; I(2), 51–79; C, 52–85<br />
Comments:<br />
A Simon design was<br />
used to calculate<br />
that a sample size <strong>of</strong><br />
130 was required to<br />
distinguish a 60%<br />
PSA response from<br />
a 30% response<br />
<strong>with</strong> 80% power<br />
and a Type 1 err<strong>or</strong><br />
<strong>of</strong> 0.05<br />
O<strong>the</strong>r participant characteristics:<br />
Time from diagnosis to random<br />
assignment (median months, IQ<br />
range):<br />
I(1): 33, 3–219<br />
I(2): 33, 5–151<br />
C: 47, 6–150<br />
I(1): 1 c<strong>or</strong>ticosteroid premedication-related death rep<strong>or</strong>ted<br />
Baseline<br />
comparability: Yes,<br />
non-significant trend<br />
f<strong>or</strong> I(2) to have<br />
better ECOG<br />
perf<strong>or</strong>mance status<br />
(p = 0.18)<br />
O<strong>the</strong>r adverse events:<br />
As<strong>the</strong>nia:<br />
Time from start <strong>of</strong> h<strong>or</strong>monal<br />
<strong>treatment</strong> to random assignment<br />
(median months, IQ range):<br />
I(1): 16, 2–116<br />
I(2): 27, 2–89<br />
C: 25, 1–118<br />
Eligibility criteria<br />
specified: Yes<br />
I(1), 47%; I(2), 41%; C, 26%<br />
p = 0.30<br />
Nail and skin toxicities:<br />
I(1) + I(2): 14%<br />
Decrease in LVEF (grade 1 <strong>or</strong> 2):<br />
C: 4 (10%)<br />
Comments about participants:<br />
Inclusion/exclusion criteria:<br />
Histologically proven metastatic<br />
adenocarcinoma <strong>of</strong> <strong>the</strong> prostate <strong>with</strong><br />
progressive disease, despite<br />
androgen deprivation. Anti-androgen<br />
<strong>with</strong>drawal and documented disease<br />
progression were required bef<strong>or</strong>e<br />
study entry. Disease progression was<br />
defined as appearance <strong>of</strong> new<br />
Co-interventions:<br />
Premedication <strong>with</strong><br />
<strong>or</strong>al <strong>prednisolone</strong>,<br />
300 mg total dose<br />
and <strong>or</strong>al warfarin<br />
2 mg/day<br />
administered<br />
continuously in I(1)<br />
and I(2)<br />
Outcome 6: Pain (n = 127)<br />
‘Clinical benefit’ was measured using <strong>the</strong> pain control and<br />
analgesic consumption indices <strong>of</strong> <strong>the</strong> McGill pain<br />
questionnaire and ECOG perf<strong>or</strong>mance status. Pain control<br />
was sc<strong>or</strong>ed from 0 (no pain) to 4 (uncontrollable pain) and<br />
<strong>the</strong> analgesic consumption was sc<strong>or</strong>ed from 0 (no<br />
requirement) to 4 (regular, narcotic analgesic use). Clinical<br />
From Oudard<br />
et al.: 38,39 coumadin<br />
(2 mg <strong>or</strong>ally) given<br />
continued