Sabato 27 ottobre 2012 - Pacini Editore
Sabato 27 ottobre 2012 - Pacini Editore
Sabato 27 ottobre 2012 - Pacini Editore
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
COmuNiCaziONi ORali<br />
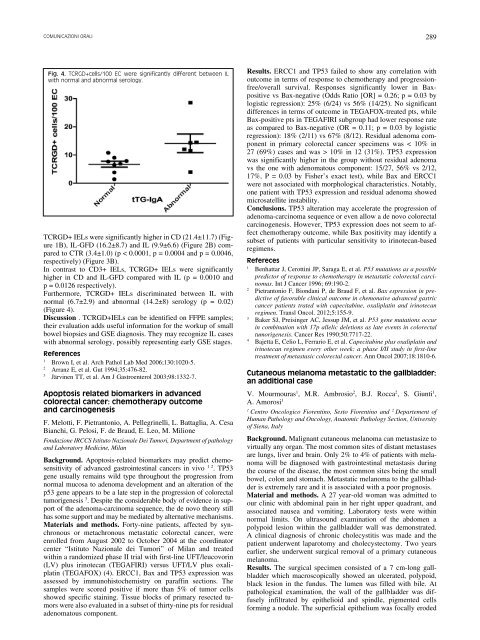
Fig. 4. tCRGd+cells/100 EC were significantly different between il<br />
with normal and abnormal serology.<br />
TCRGD+ IELs were significantly higher in CD (21.4±11.7) (Figure<br />
1B), IL-GFD (16.2±8.7) and IL (9.9±6.6) (Figure 2B) compared<br />
to CTR (3.4±1.0) (p < 0.0001, p = 0.0004 and p = 0.0046,<br />
respectively) (Figure 3B).<br />
In contrast to CD3+ IELs, TCRGD+ IELs were significantly<br />
higher in CD and IL-GFD compared with IL (p = 0.0010 and<br />
p = 0.0126 respectively).<br />
Furthermore, TCRGD+ IELs discriminated between IL with<br />
normal (6.7±2.9) and abnormal (14.2±8) serology (p = 0.02)<br />
(Figure 4).<br />
Discussion . TCRGD+IELs can be identified on FFPE samples;<br />
their evaluation adds useful information for the workup of small<br />
bowel biopsies and GSE diagnosis. They may recognize IL cases<br />
with abnormal serology, possibly representing early GSE stages.<br />
references<br />
1 Brown I, et al. Arch Pathol Lab Med 2006;130:1020-5.<br />
2 Arranz E, et al. Gut 1994;35:476-82.<br />
3 Järvinen TT, et al. Am J Gastroenterol 2003;98:1332-7.<br />
Apoptosis related biomarkers in advanced<br />
colorectal cancer: chemotherapy outcome<br />
and carcinogenesis<br />
F. Melotti, F. Pietrantonio, A. Pellegrinelli, L. Battaglia, A. Cesa<br />
Bianchi, G. Pelosi, F. de Braud, E. Leo, M. Milione<br />
Fondazione IRCCS Istituto Nazionale Dei Tumori, Department of pathology<br />
and Laboratory Medicine, Milan<br />
Background. Apoptosis-related biomarkers may predict chemosensitivity<br />
of advanced gastrointestinal cancers in vivo 1 2 . TP53<br />
gene usually remains wild type throughout the progression from<br />
normal mucosa to adenoma development and an alteration of the<br />
p53 gene appears to be a late step in the progression of colorectal<br />
tumorigenesis 3 . Despite the considerable body of evidence in support<br />
of the adenoma-carcinoma sequence, the de novo theory still<br />
has some support and may be mediated by alternative mechanisms.<br />
Materials and methods. Forty-nine patients, affected by synchronous<br />
or metachronous metastatic colorectal cancer, were<br />
enrolled from August 2002 to October 2004 at the coordinator<br />
center “Istituto Nazionale dei Tumori” of Milan and treated<br />
within a randomized phase II trial with first-line UFT/leucovorin<br />
(LV) plus irinotecan (TEGAFIRI) versus UFT/LV plus oxaliplatin<br />
(TEGAFOX) (4). ERCC1, Bax and TP53 expression was<br />
assessed by immunohistochemistry on paraffin sections. The<br />
samples were scored positive if more than 5% of tumor cells<br />
showed specific staining. Tissue blocks of primary resected tumors<br />
were also evaluated in a subset of thirty-nine pts for residual<br />
adenomatous component.<br />
289<br />
Results. ERCC1 and TP53 failed to show any correlation with<br />
outcome in terms of response to chemotherapy and progressionfree/overall<br />
survival. Responses significantly lower in Baxpositive<br />
vs Bax-negative (Odds Ratio [OR] = 0.26; p = 0.03 by<br />
logistic regression): 25% (6/24) vs 56% (14/25). No significant<br />
differences in terms of outcome in TEGAFOX-treated pts, while<br />
Bax-positive pts in TEGAFIRI subgroup had lower response rate<br />
as compared to Bax-negative (OR = 0.11; p = 0.03 by logistic<br />
regression): 18% (2/11) vs 67% (8/12). Residual adenoma component<br />
in primary colorectal cancer specimens was < 10% in<br />
<strong>27</strong> (69%) cases and was > 10% in 12 (31%). TP53 expression<br />
was significantly higher in the group without residual adenoma<br />
vs the one with adenomatous component: 15/<strong>27</strong>, 56% vs 2/12,<br />
17%, P = 0.03 by Fisher’s exact test), while Bax and ERCC1<br />
were not associated with morphological characteristics. Notably,<br />
one patient with TP53 expression and residual adenoma showed<br />
microsatellite instability.<br />
Conclusions. TP53 alteration may accelerate the progression of<br />
adenoma-carcinoma sequence or even allow a de novo colorectal<br />
carcinogenesis. However, TP53 expression does not seem to affect<br />
chemotherapy outcome, while Bax positivity may identify a<br />
subset of patients with particular sensitivity to irinotecan-based<br />
regimens.<br />
refereces<br />
1 Benhattar J, Cerottini JP, Saraga E, et al. P53 mutations as a possible<br />
predictor of response to chemotherapy in metastatic colorectal carcinomas.<br />
Int J Cancer 1996; 69:190-2.<br />
2 Pietrantonio F, Biondani P, de Braud F, et al. Bax espression in predictive<br />
of favorable clinical outcome in chemonaive advanced gastric<br />
cancer patients trated with capecitabine, oxaliplatin and irinotecan<br />
regimen. Transl Oncol. <strong>2012</strong>;5:155-9.<br />
3 Baker SJ, Preisinger AC, Jessup JM, et al. P53 gene mutations occur<br />
in combination with 17p allelic deletions as late events in colorectal<br />
tumorigenesis. Cancer Res 1990;50:7717-22.<br />
4 Bajetta E, Celio L, Ferrario E, et al. Capecitabine plus oxaliplatin and<br />
irinotecan regimen every other week: a phase I/II study in first-line<br />
treatment of metastasic colorectal cancer. Ann Oncol 2007;18:1810-6.<br />
Cutaneous melanoma metastatic to the gallbladder:<br />
an additional case<br />
V. Mourmouras1 , M.R. Ambrosio2 , B.J. Rocca2 , S. Giunti1 ,<br />
A. Amorosi1 1 2 Centro Oncologico Fiorentino, Sesto Fiorentino and Departement of<br />
Human Pathology and Oncology, Anatomic Pathology Section, University<br />
of Siena, Italy<br />
Background. Malignant cutaneous melanoma can metastasize to<br />
virtually any organ. The most common sites of distant metastases<br />
are lungs, liver and brain. Only 2% to 4% of patients with melanoma<br />
will be diagnosed with gastrointestinal metastasis during<br />
the course of the disease, the most common sites being the small<br />
bowel, colon and stomach. Metastatic melanoma to the gallbladder<br />
is extremely rare and it is associated with a poor prognosis.<br />
Material and methods. A <strong>27</strong> year-old woman was admitted to<br />
our clinic with abdominal pain in her right upper quadrant, and<br />
associated nausea and vomiting. Laboratory tests were within<br />
normal limits. On ultrasound examination of the abdomen a<br />
polypoid lesion within the gallbladder wall was demonstrated.<br />
A clinical diagnosis of chronic cholecystitis was made and the<br />
patient underwent laparotomy and cholecystectomy. Two years<br />
earlier, she underwent surgical removal of a primary cutaneous<br />
melanoma.<br />
Results. The surgical specimen consisted of a 7 cm-long gallbladder<br />
which macroscopically showed an ulcerated, polypoid,<br />
black lesion in the fundus. The lumen was filled with bile. At<br />
pathological examination, the wall of the gallbladder was diffusely<br />
infiltrated by epithelioid and spindle, pigmented cells<br />
forming a nodule. The superficial epithelium was focally eroded