The Implementation of a Model of Person-Centred Practice In Older ...
The Implementation of a Model of Person-Centred Practice In Older ...
The Implementation of a Model of Person-Centred Practice In Older ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>The</strong> implementation <strong>of</strong> a model <strong>of</strong> person-centred practice in older person settings<br />
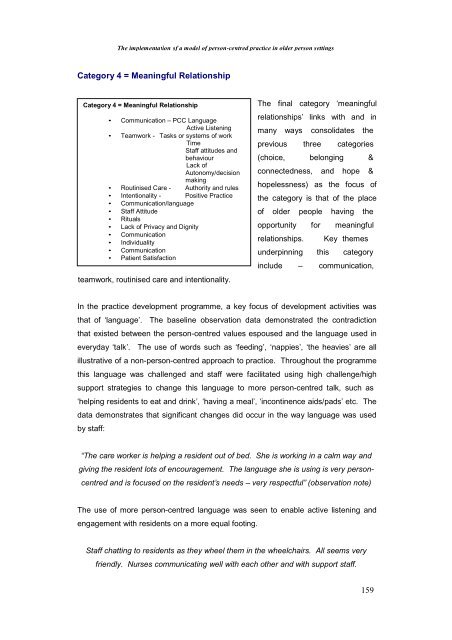
Category 4 = Meaningful Relationship<br />
Category 4 = Meaningful Relationship<br />
• Communication – PCC Language<br />
Active Listening<br />
• Teamwork - Tasks or systems <strong>of</strong> work<br />
Time<br />
Staff attitudes and<br />
behaviour<br />
Lack <strong>of</strong><br />
Autonomy/decision<br />
making<br />
• Routinised Care - Authority and rules<br />
• <strong>In</strong>tentionality - Positive <strong>Practice</strong><br />
• Communication/language<br />
• Staff Attitude<br />
• Rituals<br />
• Lack <strong>of</strong> Privacy and Dignity<br />
• Communication<br />
• <strong>In</strong>dividuality<br />
• Communication<br />
• Patient Satisfaction<br />
teamwork, routinised care and intentionality.<br />
<strong>The</strong> final category ‘meaningful<br />
relationships’ links with and in<br />
many ways consolidates the<br />
previous three categories<br />
(choice, belonging &<br />
connectedness, and hope &<br />
hopelessness) as the focus <strong>of</strong><br />
the category is that <strong>of</strong> the place<br />
<strong>of</strong> older people having the<br />
opportunity for meaningful<br />
relationships. Key themes<br />
underpinning this category<br />
include – communication,<br />
<strong>In</strong> the practice development programme, a key focus <strong>of</strong> development activities was<br />
that <strong>of</strong> ‘language’. <strong>The</strong> baseline observation data demonstrated the contradiction<br />
that existed between the person-centred values espoused and the language used in<br />
everyday ‘talk’. <strong>The</strong> use <strong>of</strong> words such as ‘feeding’, ‘nappies’, ‘the heavies’ are all<br />
illustrative <strong>of</strong> a non-person-centred approach to practice. Throughout the programme<br />
this language was challenged and staff were facilitated using high challenge/high<br />
support strategies to change this language to more person-centred talk, such as<br />
‘helping residents to eat and drink’, ‘having a meal’, ‘incontinence aids/pads’ etc. <strong>The</strong><br />
data demonstrates that significant changes did occur in the way language was used<br />
by staff:<br />
“<strong>The</strong> care worker is helping a resident out <strong>of</strong> bed. She is working in a calm way and<br />
giving the resident lots <strong>of</strong> encouragement. <strong>The</strong> language she is using is very person-<br />
centred and is focused on the resident’s needs – very respectful” (observation note)<br />
<strong>The</strong> use <strong>of</strong> more person-centred language was seen to enable active listening and<br />
engagement with residents on a more equal footing.<br />
Staff chatting to residents as they wheel them in the wheelchairs. All seems very<br />
friendly. Nurses communicating well with each other and with support staff.<br />
159