6th European Conference - Academic Conferences
6th European Conference - Academic Conferences
6th European Conference - Academic Conferences
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
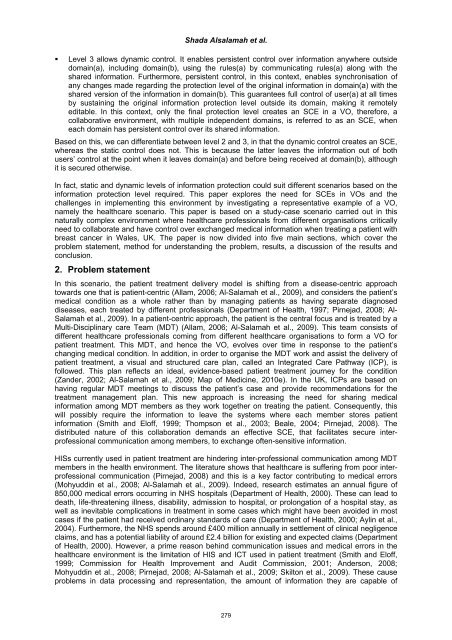
Shada Alsalamah et al.<br />
Level 3 allows dynamic control. It enables persistent control over information anywhere outside<br />
domain(a), including domain(b), using the rules(a) by communicating rules(a) along with the<br />
shared information. Furthermore, persistent control, in this context, enables synchronisation of<br />
any changes made regarding the protection level of the original information in domain(a) with the<br />
shared version of the information in domain(b). This guarantees full control of user(a) at all times<br />
by sustaining the original information protection level outside its domain, making it remotely<br />
editable. In this context, only the final protection level creates an SCE in a VO, therefore, a<br />
collaborative environment, with multiple independent domains, is referred to as an SCE, when<br />
each domain has persistent control over its shared information.<br />
Based on this, we can differentiate between level 2 and 3, in that the dynamic control creates an SCE,<br />
whereas the static control does not. This is because the latter leaves the information out of both<br />
users’ control at the point when it leaves domain(a) and before being received at domain(b), although<br />
it is secured otherwise.<br />
In fact, static and dynamic levels of information protection could suit different scenarios based on the<br />
information protection level required. This paper explores the need for SCEs in VOs and the<br />
challenges in implementing this environment by investigating a representative example of a VO,<br />
namely the healthcare scenario. This paper is based on a study-case scenario carried out in this<br />
naturally complex environment where healthcare professionals from different organisations critically<br />
need to collaborate and have control over exchanged medical information when treating a patient with<br />
breast cancer in Wales, UK. The paper is now divided into five main sections, which cover the<br />
problem statement, method for understanding the problem, results, a discussion of the results and<br />
conclusion.<br />
2. Problem statement<br />
In this scenario, the patient treatment delivery model is shifting from a disease-centric approach<br />
towards one that is patient-centric (Allam, 2006; Al-Salamah et al., 2009), and considers the patient’s<br />
medical condition as a whole rather than by managing patients as having separate diagnosed<br />
diseases, each treated by different professionals (Department of Health, 1997; Pirnejad, 2008; Al-<br />
Salamah et al., 2009). In a patient-centric approach, the patient is the central focus and is treated by a<br />
Multi-Disciplinary care Team (MDT) (Allam, 2006; Al-Salamah et al., 2009). This team consists of<br />
different healthcare professionals coming from different healthcare organisations to form a VO for<br />
patient treatment. This MDT, and hence the VO, evolves over time in response to the patient’s<br />
changing medical condition. In addition, in order to organise the MDT work and assist the delivery of<br />
patient treatment, a visual and structured care plan, called an Integrated Care Pathway (ICP), is<br />
followed. This plan reflects an ideal, evidence-based patient treatment journey for the condition<br />
(Zander, 2002; Al-Salamah et al., 2009; Map of Medicine, 2010e). In the UK, ICPs are based on<br />
having regular MDT meetings to discuss the patient’s case and provide recommendations for the<br />
treatment management plan. This new approach is increasing the need for sharing medical<br />
information among MDT members as they work together on treating the patient. Consequently, this<br />
will possibly require the information to leave the systems where each member stores patient<br />
information (Smith and Eloff, 1999; Thompson et al., 2003; Beale, 2004; Pirnejad, 2008). The<br />
distributed nature of this collaboration demands an effective SCE, that facilitates secure interprofessional<br />
communication among members, to exchange often-sensitive information.<br />
HISs currently used in patient treatment are hindering inter-professional communication among MDT<br />
members in the health environment. The literature shows that healthcare is suffering from poor interprofessional<br />
communication (Pirnejad, 2008) and this is a key factor contributing to medical errors<br />
(Mohyuddin et al., 2008; Al-Salamah et al., 2009). Indeed, research estimates an annual figure of<br />
850,000 medical errors occurring in NHS hospitals (Department of Health, 2000). These can lead to<br />
death, life-threatening illness, disability, admission to hospital, or prolongation of a hospital stay, as<br />
well as inevitable complications in treatment in some cases which might have been avoided in most<br />
cases if the patient had received ordinary standards of care (Department of Health, 2000; Aylin et al.,<br />
2004). Furthermore, the NHS spends around £400 million annually in settlement of clinical negligence<br />
claims, and has a potential liability of around £2.4 billion for existing and expected claims (Department<br />
of Health, 2000). However, a prime reason behind communication issues and medical errors in the<br />
healthcare environment is the limitation of HIS and ICT used in patient treatment (Smith and Eloff,<br />
1999; Commission for Health Improvement and Audit Commission, 2001; Anderson, 2008;<br />
Mohyuddin et al., 2008; Pirnejad, 2008; Al-Salamah et al., 2009; Skilton et al., 2009). These cause<br />
problems in data processing and representation, the amount of information they are capable of<br />
279