Invasive breast carcinoma - IARC
Invasive breast carcinoma - IARC
Invasive breast carcinoma - IARC
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
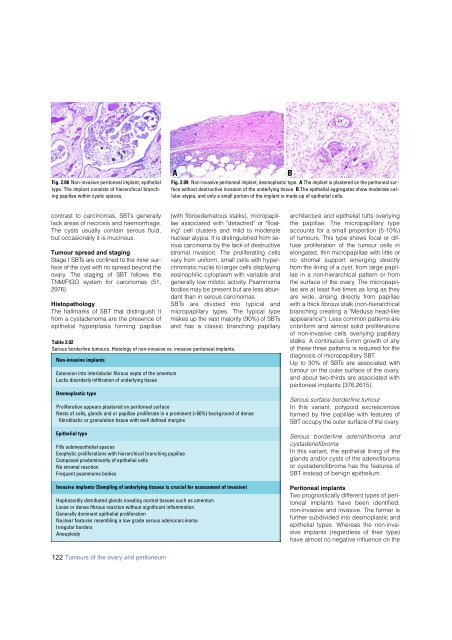
Fig. 2.08 Non-invasive peritoneal implant, epithelial<br />
type. The implant consists of hierarchical branching<br />
papillae within cystic spaces.<br />
A<br />
Fig. 2.09 Non-invasive peritoneal implant, desmoplastic type. A The implant is plastered on the peritoneal sur -<br />
face without destructive invasion of the underlying tissue. B The epithelial aggregates show moderate cellular<br />
atypia, and only a small portion of the implant is made up of epithelial cells.<br />
B<br />
contrast to <strong>carcinoma</strong>s, SBTs generally<br />
lack areas of necrosis and haemorrhage.<br />
The cysts usually contain serous fluid,<br />
but occasionally it is mucinous.<br />
Tumour spread and staging<br />
Stage I SBTs are confined to the inner surface<br />
of the cyst with no spread beyond the<br />
o v a ry. The staging of SBT follows the<br />
TNM/FIGO system for <strong>carcinoma</strong>s {51,<br />
2 9 7 6 } .<br />
Histopathology<br />
The hallmarks of SBT that distinguish it<br />
f rom a cystadenoma are the presence of<br />
epithelial hyperplasia forming papillae<br />
(with fibroedematous stalks), micro p a p i l-<br />
lae associated with "detached" or "floating"<br />
cell clusters and mild to moderate<br />
nuclear atypia. It is distinguished from serous<br />
<strong>carcinoma</strong> by the lack of destructive<br />
s t romal invasion. The proliferating cells<br />
v a ry from uniform, small cells with hyperc<br />
h romatic nuclei to larger cells displaying<br />
eosinophilic cytoplasm with variable and<br />
generally low mitotic activity. Psammoma<br />
bodies may be present but are less abundant<br />
than in serous carc i n o m a s .<br />
S B Ts are divided into typical and<br />
m i c ro p a p i l l a ry types. The typical type<br />
makes up the vast majority (90%) of SBTs<br />
and has a classic branching papillary<br />
Table 2.02<br />
Serous borderline tumours. Histology of non-invasive vs. invasive peritoneal implants.<br />
Non-invasive implants<br />
Extension into interlobular fibrous septa of the omentum<br />
Lacks disorderly infiltration of underlying tissue<br />
Desmoplastic type<br />
Proliferation appears plastered on peritoneal surface<br />
Nests of cells, glands and or papillae proliferate in a prominent (>50%) background of dense<br />
fibroblastic or granulation tissue with well defined margins<br />
Epithelial type<br />
Fills submesothelial spaces<br />
Exophytic proliferations with hierarchical branching papillae<br />
Composed predominantly of epithelial cells<br />
No stromal reaction<br />
Frequent psammoma bodies<br />
<strong>Invasive</strong> implants (Sampling of underlying tissues is crucial for assessment of invasion)<br />
Haphazardly distributed glands invading normal tissues such as omentum<br />
Loose or dense fibrous reaction without significant inflammation<br />
Generally dominant epithelial proliferation<br />
Nuclear features resembling a low grade serous adeno<strong>carcinoma</strong><br />
Irregular borders<br />
Aneuploidy<br />
a rc h i t e c t u re and epithelial tufts overlying<br />
the papillae. The micro p a p i l l a ry type<br />
accounts for a small pro p o rtion (5-10%)<br />
of tumours. This type shows focal or diffuse<br />
proliferation of the tumour cells in<br />
elongated, thin micropapillae with little or<br />
no stromal support emerging dire c t l y<br />
f rom the lining of a cyst, from large papillae<br />
in a non-hierarchical pattern or fro m<br />
the surface of the ovary. The micro p a p i l-<br />
lae are at least five times as long as they<br />
a re wide, arising directly from papillae<br />
with a thick fibrous stalk (non-hierarc h i c a l<br />
branching creating a "Medusa head-like<br />
appearance"). Less common patterns are<br />
c r i b r i f o rm and almost solid pro l i f e r a t i o n s<br />
of non-invasive cells overlying papillary<br />
stalks. A continuous 5-mm growth of any<br />
of these three patterns is re q u i red for the<br />
diagnosis of micro p a p i l l a ry SBT.<br />
Up to 30% of SBTs are associated with<br />
tumour on the outer surface of the ovary,<br />
and about two-thirds are associated with<br />
peritoneal implants {376,2615}.<br />
Serous surface borderline tumour<br />
In this variant, polypoid excrescences<br />
formed by fine papillae with features of<br />
SBT occupy the outer surface of the ovary.<br />
S e rous borderline adenofibroma and<br />
cystadenofibroma<br />
In this variant, the epithelial lining of the<br />
glands and/or cysts of the adenofibroma<br />
or cystadenofibroma has the features of<br />
SBT instead of benign epithelium.<br />
Peritoneal implants<br />
Two prognostically different types of peritoneal<br />
implants have been identified,<br />
non-invasive and invasive. The former is<br />
further subdivided into desmoplastic and<br />
epithelial types. Whereas the non-invasive<br />
implants (regardless of their type)<br />
have almost no negative influence on the<br />
122 Tumours of the ovary and peritoneum