Invasive breast carcinoma - IARC
Invasive breast carcinoma - IARC
Invasive breast carcinoma - IARC
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
A<br />
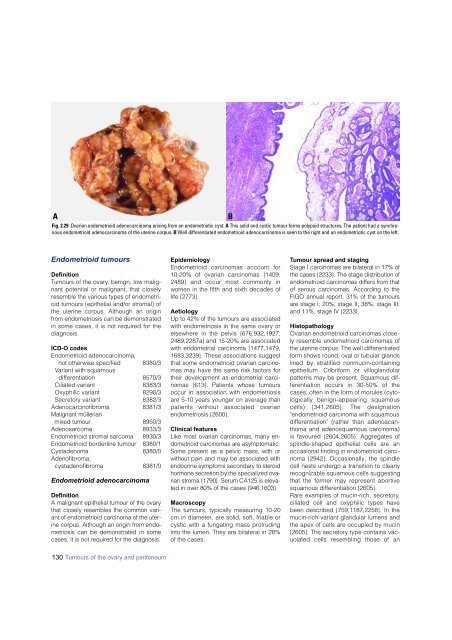
Fig. 2.29 Ovarian endometrioid adeno<strong>carcinoma</strong> arising from an endometriotic cyst. A This solid and cystic tumour forms polypoid structures. The patient had a synchronous<br />
endometrioid adeno<strong>carcinoma</strong> of the uterine corpus. B Well differentiated endometrioid adeno<strong>carcinoma</strong> is seen to the right and an endometriotic cyst on the left.<br />
B<br />
Endometrioid tumours<br />
Definition<br />
Tumours of the ovary, benign, low malignant<br />
potential or malignant, that closely<br />
resemble the various types of endometrioid<br />
tumours (epithelial and/or stromal) of<br />
the uterine corpus. Although an origin<br />
from endometriosis can be demonstrated<br />
in some cases, it is not required for the<br />
diagnosis.<br />
ICD-O codes<br />
Endometrioid adeno<strong>carcinoma</strong>,<br />
not otherwise specified 8380/3<br />
Variant with squamous<br />
differentiation 8570/3<br />
Ciliated variant 8383/3<br />
Oxyphilic variant 8290/3<br />
Secretory variant 8382/3<br />
Adenocarcinofibroma 8381/3<br />
Malignant müllerian<br />
mixed tumour 8950 / 3<br />
Adenosarcoma 8933/3<br />
Endometrioid stromal sarcoma 8930/3<br />
Endometrioid borderline tumour 8380/1<br />
Cystadenoma 8380/0<br />
Adenofibroma;<br />
cystadenofibroma 8381/0<br />
Endometrioid adeno<strong>carcinoma</strong><br />
Definition<br />
A malignant epithelial tumour of the ovary<br />
that closely resembles the common variant<br />
of endometrioid <strong>carcinoma</strong> of the uterine<br />
corpus. Although an origin from endometriosis<br />
can be demonstrated in some<br />
cases, it is not re q u i red for the diagnosis.<br />
Epidemiology<br />
Endometrioid <strong>carcinoma</strong>s account for<br />
10-20% of ovarian <strong>carcinoma</strong>s {1409,<br />
2489} and occur most commonly in<br />
women in the fifth and sixth decades of<br />
life {2773}.<br />
Aetiology<br />
Up to 42% of the tumours are associated<br />
with endometriosis in the same ovary or<br />
elsewhere in the pelvis {676,932,1927,<br />
2489,2287a} and 15-20% are associated<br />
with endometrial <strong>carcinoma</strong> {1477,1479,<br />
1683,3239}. These associations suggest<br />
that some endometrioid ovarian <strong>carcinoma</strong>s<br />
may have the same risk factors for<br />
their development as endometrial <strong>carcinoma</strong>s<br />
{613}. Patients whose tumours<br />
occur in association with endometriosis<br />
are 5-10 years younger on average than<br />
patients without associated ovarian<br />
endometriosis {2600}.<br />
Clinical features<br />
Like most ovarian <strong>carcinoma</strong>s, many endometrioid<br />
<strong>carcinoma</strong>s are asymptomatic.<br />
Some present as a pelvic mass, with or<br />
without pain and may be associated with<br />
endocrine symptoms secondary to stero i d<br />
h o rmone secretion by the specialized ovarian<br />
stroma {1790}. Serum CA125 is elevated<br />
in over 80% of the cases {946,1603}.<br />
Macroscopy<br />
The tumours, typically measuring 10-20<br />
cm in diameter, are solid, soft, friable or<br />
cystic with a fungating mass protruding<br />
into the lumen. They are bilateral in 28%<br />
of the cases.<br />
Tumour spread and staging<br />
Stage I <strong>carcinoma</strong>s are bilateral in 17% of<br />
the cases {2233}. The stage distribution of<br />
endometrioid <strong>carcinoma</strong>s differs from that<br />
of serous <strong>carcinoma</strong>s. According to the<br />
FIGO annual re p o rt, 31% of the tumours<br />
a re stage I; 20%, stage II; 38%, stage III;<br />
and 11%, stage IV {2233}.<br />
Histopathology<br />
Ovarian endometrioid <strong>carcinoma</strong>s closely<br />
resemble endometrioid <strong>carcinoma</strong>s of<br />
the uterine corpus. The well differentiated<br />
form shows round, oval or tubular glands<br />
lined by stratified nonmucin-containing<br />
epithelium. Cribriform or villoglandular<br />
patterns may be present. Squamous diff<br />
e rentiation occurs in 30-50% of the<br />
cases, often in the form of morules (cytologically<br />
benign-appearing squamous<br />
cells) {341,2605}. The designation<br />
"endometrioid <strong>carcinoma</strong> with squamous<br />
differentiation" (rather than adenoacanthoma<br />
and adenosquamous <strong>carcinoma</strong>)<br />
is favoured {2604,2605}. Aggregates of<br />
spindle-shaped epithelial cells are an<br />
occasional finding in endometrioid <strong>carcinoma</strong><br />
{2942}. Occasionally, the spindle<br />
cell nests undergo a transition to clearly<br />
recognizable squamous cells suggesting<br />
that the former may represent abortive<br />
squamous differentiation {2605}.<br />
Rare examples of mucin-rich, secretory,<br />
ciliated cell and oxyphilic types have<br />
been described {759,1187,2258}. In the<br />
mucin-rich variant glandular lumens and<br />
the apex of cells are occupied by mucin<br />
{2605}. The secretory type contains vacuolated<br />
cells resembling those of an<br />
130 Tumours of the ovary and peritoneum