Invasive breast carcinoma - IARC
Invasive breast carcinoma - IARC
Invasive breast carcinoma - IARC
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
unusual variants as well. Using this<br />
approach many apocrine DCIS lesions<br />
qualify as high grade, while a minority<br />
would qualify as intermediate or, rarely,<br />
high grade DCIS. The clear and spindle<br />
cell DCIS are sometimes found coexistent<br />
and continuous with typical low<br />
grade DCIS, but often the nuclei are<br />
moderately atypical qualifying the<br />
lesions as intermediate grade DCIS.<br />
High nuclear grade spindle or clear cell<br />
DCIS is extremely rare. A vast majority of<br />
apocrine <strong>carcinoma</strong>s are ER, PR and<br />
BCL2 negative, but androgen receptor<br />
positive {2888}.<br />
Proliferation<br />
In vivo labelling with bromodeoxyuridine<br />
(BrdU) has found no significant differences<br />
between proliferating cell fraction<br />
among UDH and ADH, but the proliferating<br />
cell fraction is significantly increased<br />
in DCIS {412}. With the Ki67 antibody, the<br />
highest proliferating index (PI) of 13%<br />
has been noted among the comedo<br />
DCIS, while the PI for low grade DCIS,<br />
cribriform type is 4.5% and for micropapillary<br />
type, it is 0% {61}.<br />
DNA Ploidy: Aneuploidy has been found<br />
in 7% of UDH, 13-36% of ADH, and 30-<br />
72% of low to high grade DCIS respectively<br />
{408,579,792}.<br />
Hormone receptor expression<br />
E s t rogen plays a central role in re g u l a t i n g<br />
the growth and diff e rentiation of bre a s t<br />
epithelium as well as in the expression of<br />
other genes including the pro g e s t e ro n e<br />
receptor (PR) {72}. The presence and<br />
concentration of the two receptors are<br />
used, not only as a clinical index of<br />
potential therapeutic response, but also<br />
as markers of prognosis for invasive<br />
b reast <strong>carcinoma</strong>s {196}. Only a few<br />
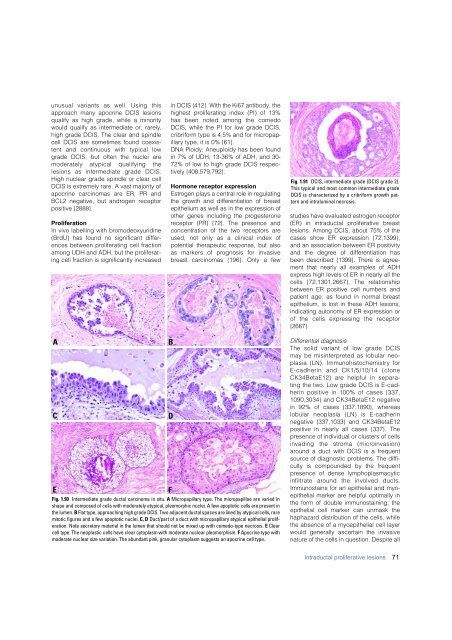
Fig. 1.91 DCIS, intermediate grade (DCIS grade 2).<br />
This typical and most common intermediate grade<br />
DCIS is characterized by a cribriform growth pattern<br />
and intraluminal necrosis.<br />
studies have evaluated estrogen re c e p t o r<br />
(ER) in intraductal proliferative bre a s t<br />
lesions. Among DCIS, about 75% of the<br />
cases show ER expression {72,1399},<br />
and an association between ER positivity<br />
and the degree of diff e rentiation has<br />
been described {1399}. There is agre e-<br />
ment that nearly all examples of ADH<br />
e x p ress high levels of ER in nearly all the<br />
cells {72,1301,2667}. The re l a t i o n s h i p<br />
between ER positive cell numbers and<br />
patient age, as found in normal bre a s t<br />
epithelium, is lost in these ADH lesions,<br />
indicating autonomy of ER expression or<br />
of the cells expressing the re c e p t o r<br />
{ 2 6 6 7 } .<br />
A<br />
C<br />
E<br />
F<br />
Fig. 1.90 Intermediate grade ductal <strong>carcinoma</strong> in situ. A Micropapillary type. The micropapillae are varied in<br />
shape and composed of cells with moderately atypical, pleomorphic nuclei. A few apoptotic cells are present in<br />
the lumen. B Flat type, approaching high grade DCIS. Two adjacent ductal spaces are lined by atypical cells, rare<br />
mitotic figures and a few apoptotic nuclei. C, D Duct/part of a duct with micropapillary atypical epithelial proliferation.<br />
Note secretory material in the lumen that should not be mixed up with comedo-type necrosis. E C l e a r<br />
cell type. The neoplastic cells have clear cytoplasm with moderate nuclear pleomorphism. F Apocrine type with<br />
moderate nuclear size variation. The abundant pink, granular cytoplasm suggests an apocrine cell type.<br />
B<br />
D<br />
Differential diagnosis<br />
The solid variant of low grade DCIS<br />
may be misinterpreted as lobular neoplasia<br />
(LN). Immunohistochemistry for<br />
E-cadherin and CK1/5/10/14 (clone<br />
CK34BetaE12) are helpful in separating<br />
the two. Low grade DCIS is E-cadherin<br />
positive in 100% of cases {337,<br />
1090,3034} and CK34BetaE12 negative<br />
in 92% of cases {337,1890}, whereas<br />
lobular neoplasia (LN) is E-cadherin<br />
negative {337,1033} and CK34BetaE12<br />
positive in nearly all cases {337}. The<br />
presence of individual or clusters of cells<br />
invading the stroma (micro i n v a s i o n )<br />
around a duct with DCIS is a frequent<br />
source of diagnostic problems. The difficulty<br />
is compounded by the frequent<br />
presence of dense lymphoplasmacytic<br />
infiltrate around the involved ducts.<br />
Immunostains for an epithelial and myoepithelial<br />
marker are helpful optimally in<br />
the form of double immunostaining; the<br />
epithelial cell marker can unmask the<br />
haphazard distribution of the cells, while<br />
the absence of a myoepithelial cell layer<br />
would generally ascertain the invasive<br />
nature of the cells in question. Despite all<br />
Intraductal proliferative lesions<br />
71