Invasive breast carcinoma - IARC
Invasive breast carcinoma - IARC
Invasive breast carcinoma - IARC
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Histopathology<br />
This epithelial tumour may show diffuse,<br />
solid tubular, hollow tubular and sievelike<br />
patterns, and combinations of the<br />
various patterns may occur. Cases have<br />
been reported associated with endometrial<br />
hyperplasia {1262,1289}.<br />
Immunoprofile<br />
The neoplasms are positive for CAM5.2,<br />
cytokeratins 7 and 19 and vimentin but<br />
a re negative for cytokeratin 20,<br />
34betaE12, B72.3, carc i n o e m b ry o n i c<br />
antigen, and epithelial membrane antigen<br />
{2321,2878,2926}. The neoplastic cells<br />
often express CD10 {2110} and often are<br />
weakly positive for alpha-inhibin {1499}.<br />
Histogenesis<br />
Cases have been reported arising within<br />
the rete ovarii {662,2878}. An immunohistochemical<br />
study based on a comparison<br />
with mesonephric remnants and<br />
paramesonephric structures supported<br />
but did not prove a mesonephric origin of<br />
these neoplasms {2926}.<br />
Prognosis and predictive factors<br />
These tumours typically are not aggressive;<br />
however, a significant minority of<br />
patients have had an aggressive course<br />
{3212}. The malignant cases sometimes,<br />
but not always, show nuclear atypia and<br />
increased mitotic activity.<br />
Wilms tumour<br />
Definition<br />
A primary ovarian neoplasm that has the<br />
typical features of a Wilms tumour of the<br />
kidney.<br />
Epidemiology<br />
Several cases of pure Wilms tumour of the<br />
o v a ry have been re p o rted {1303,2506}.<br />
Clinical features<br />
The tumour occurs in patients in the re p roductive<br />
age group and beyond and pre s-<br />
ents as a rapidly growing adnexal mass.<br />
Histopathology<br />
They have the typical appearance of a<br />
Wilms tumour including small tubules,<br />
glomeruloid structures and blastema. No<br />
teratomatous elements were identified.<br />
Prognosis and predictive factors<br />
Two of the patients were living and well<br />
10 months and 7 years postoperatively.<br />
Paraganglioma<br />
Definition<br />
A unique neuroendocrine neoplasm,<br />
usually encapsulated and benign, arising<br />
in specialized neural crest cells associated<br />
with autonomic ganglia (paraganglia).<br />
Synonym<br />
Phaeochromocytoma.<br />
Clinical features<br />
A single case of a paraganglioma of the<br />
ovary in a fifteen year old girl with hypertension<br />
has been reported {832}. In addition<br />
two unpublished cases have been<br />
described {2605}.<br />
Histopathology<br />
The tumours consist of polygonal epithelioid<br />
cells arranged in nests separated by<br />
a fibrovascular stroma.<br />
Immunoprofile<br />
The tumour is positive for chromogranin.<br />
In addition, stains for S-100 protein can<br />
identify sustentacular cells {2605}.<br />
Biochemistry<br />
Epinephrine and norepinephrine were<br />
extracted from the tumour {832}.<br />
Myxoma<br />
Definition<br />
A benign mesenchymal tumour composed<br />
of cells with bland nuclear feat<br />
u res producing abundant basophilic<br />
intercellular ground substance.<br />
Clinical features<br />
Patients with ovarian myxomas present in<br />
the reproductive age group typically with<br />
an asymptomatic unilateral adnexal<br />
mass {757}.<br />
Macrosocopy<br />
The tumours are large, averaging 11 cm<br />
in diameter. The sectioned surface is<br />
soft, often with cystic degeneration.<br />
Histopathology<br />
Myxoma is a sharply demarcated tumour<br />
composed of spindle and stellate-shaped<br />
cells within an abundant, well vascularized<br />
myxoid background. Small foci of<br />
non-myxoid fibrous tissue or smooth muscle<br />
may be present. Lipoblasts are not<br />
identified. Mitoses are rare. The interc e l-<br />
lular material stains with alcian blue and<br />
colloidal iron. Staining is prevented by<br />
p re t reatment with hyaluronidase indicating<br />
that the material is hyaluronic acid.<br />
Immunoprofile<br />
Immunohistochemical stains show that<br />
the tumours are positive for vimentin and<br />
smooth muscle actin but negative for<br />
most other common immunohistochemical<br />
markers {567}.<br />
Electron microscopy<br />
Ultrastructural features of thin filaments<br />
condensed into dense bodies also support<br />
the presence of myofibroblasts {567}.<br />
Histogenesis<br />
Based on an immunohistochemical comparison<br />
with myxoid areas of ovarian stromal<br />
tumours, myxomas were considere d<br />
to be a variant of the thecoma-fibro m a<br />
g roup {3254}.<br />
Prognosis and predictive factors<br />
The tumour is practically always benign<br />
although one case diagnosed originally<br />
as myxoma had a late recurrence after<br />
19 years {2901}. In that case the original<br />
tumour showed occasional mitotic figures<br />
(less than 1 per ten high power<br />
fields), slight atypia and occasional vacuolated<br />
cells. The recurrent neoplasm,<br />
but not the original, was aneuploid by<br />
DNA-flow cytometry {2901}.<br />
Malignant soft tissue tumours not<br />
specific to the ovary<br />
Pure soft tissue sarcomas of somatic<br />
type rarely occur as primary tumours of<br />
the ovary. They typically present as a<br />
rapidly enlarging adnexal mass. Their<br />
histological appearance is similar to soft<br />
tissue tumours in other locations. Among<br />
the reported cases of pure sarcomas are<br />
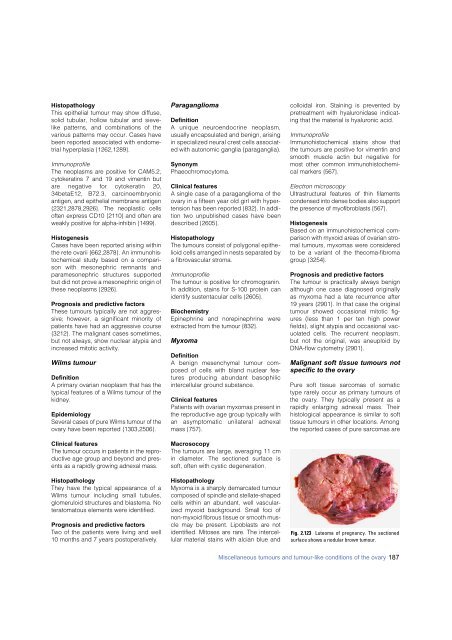
Fig. 2.123 Luteoma of pregnancy. The sectioned<br />
surface shows a nodular brown tumour.<br />
Miscellaneous tumours and tumour-like conditions of the ovary 187