The SRA Symposium - College of Medicine
The SRA Symposium - College of Medicine
The SRA Symposium - College of Medicine
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Papers<br />
sponsors must have some idea <strong>of</strong> what they expect (hope?) the experimental drug will accomplish.<br />
While researchers walk a fine line between informing vs misleading subjects about possible benefits,<br />
how can subjects make an informed decision if they can’t compare specific risks and specific<br />
benefits?<br />
But deciding to be in a clinical trial requires that subjects understand the risks and benefits <strong>of</strong> being<br />
in that trail. But if risks and benefits are not clearly articulated, how can patients be expected<br />
to make an informed decision? Although risks are <strong>of</strong>ten described as “common,” “uncommon” or<br />
“rare,” unless those terms are defined, patients will make their own definitions. Berry, et al (2003)<br />
compared the frequency <strong>of</strong> drug-related adverse events by study participants to the frequencies<br />
defined by the European Commission (EC) for events that were “very common,” “common,”<br />
“uncommon,” “rare,” or “very rare.” In every case the study participants rated the risks as likely<br />
to be more frequent than the EC definition. For example, while the EC defined a “very common”<br />
adverse event as one that affected more than 10% <strong>of</strong> patients, study participants defined “very<br />
common” as one affecting 65% <strong>of</strong> patients. <strong>The</strong> EC defined as “rare” an adverse event that affected<br />
.01% - .1% <strong>of</strong> patients, but the study participants defined “rare” as an adverse event that affected<br />
8% <strong>of</strong> patients. <strong>The</strong> point made by both <strong>of</strong> these studies is that unless risks and benefits are explicitly<br />
defined in measurable ways, patients will be unable to made an informed decision, because<br />
that decision will be based on incomplete or even missing definitions <strong>of</strong> risk and benefits.<br />
Conventional thinking implies that if only patients could better understand the consent form,<br />
they would use that understanding to make an “informed decision” about whether to volunteer to<br />
be in a clinical trial or not. But beyond that simplistic assumption, the regulatory and bioethical<br />
literature does not address the specifics <strong>of</strong> how patients actually make that kind <strong>of</strong> decision—even<br />
though there is considerable psychological research on how people make decision, especially under<br />
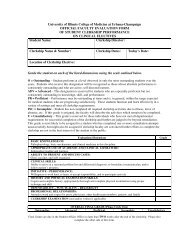
conditions <strong>of</strong> uncertainty. Table #2 summarizes five strategies that can be used by subjects to<br />
arrive at a decision—whether they understand the consent process or not.<br />
Table #2: Decision-making strategies for informed consent<br />
Decision-making strategies Explanation<br />
1. Brain anatomy 1. Informed consent takes place in the brain<br />
2. Logic and emotion 2. Brain includes areas for logical analysis and<br />
emotional reactions<br />
3. Intuition 3. Fast, selective unconscious thinking<br />
4. Heuristics 5. Mental shortcuts to reduce uncertainty or<br />
information overload<br />
5. Cognitive illusions 6. Decisions affected by how information is<br />
“framed”<br />
All decision-making strategies are based on how the brain processes specific information about a<br />
clinical trial from the consent process/consent form, as well as patients’ experiences in the health<br />
care system, their patient-doctor relationship, etc.<br />
1) Brain anatomy: Obviously informed consent takes place in the brain (Hochhauser, 2005). While<br />
the importance <strong>of</strong> the brain functioning is usually acknowledged if a clinical trial involves subjects<br />
with schizophrenia, or elderly patients with dementia, or unconscious emergency patients, the<br />
role <strong>of</strong> how the brain processes information in patients without those obvious brain disorders is<br />
seldom recognized. Federal regulators, bioethicists, and consent researchers won’t understand the<br />
consent process unless they understand how the brain processes complex information.<br />
110 2005 <strong>Symposium</strong> Proceedings Book