- Page 1 and 2:
Blue Cross and Blue Shield of Minne
- Page 3 and 4:
Recent Chapter changes: Chapter 11
- Page 5 and 6:
Chapter 11 - Coding Policies and Gu
- Page 7 and 8:
Durable Medical Equipment Date Topi
- Page 9 and 10:
Medical Emergency Date Topic Change
- Page 11 and 12:
Rehabilitative Services Date Topic
- Page 13 and 14:
Table of Contents Chapter 1 At Your
- Page 15 and 16:
Introduction Provider Policy and Pr
- Page 17 and 18:
How to Contact Us At Your Service P
- Page 19 and 20:
At Your Service Claims Address Subm
- Page 21 and 22:
Care Management Numbers and Address
- Page 23 and 24:
Care Management Numbers and Address
- Page 25 and 26:
Company Phone Number Address Public
- Page 27 and 28:
At Your Service Provider Identifica
- Page 29 and 30:
ID Cards At Your Service Introducti
- Page 31 and 32:
Electronic Commerce Overview An imp
- Page 33 and 34:
Remote Access Services (continued)
- Page 35 and 36:
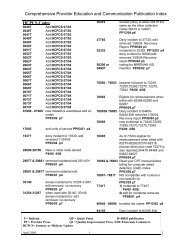
Provider Communications Provider Co
- Page 37 and 38:
Health Plan Members have the Follow
- Page 39 and 40:
Provider Agreements Participation a
- Page 41 and 42:
Provider Agreements Responsibilitie
- Page 43 and 44:
Provider Agreements Provider Number
- Page 45 and 46:
Provider Agreements Accounting for
- Page 47 and 48:
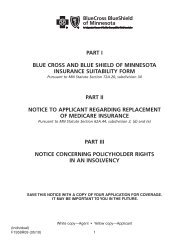
Provider Agreements Carrier Replace
- Page 49 and 50:
Table of Contents Chapter 3 Quality
- Page 51 and 52:
Quality Improvement Leadership Rati
- Page 53 and 54:
Quality Improvement Telephone Care:
- Page 55 and 56:
Quality Improvement Quality of Care
- Page 57 and 58:
Quality Improvement Written Policie
- Page 59 and 60:
Quality Improvement Written Policie
- Page 61 and 62:
Quality Improvement Patient Safety
- Page 63 and 64:
Quality Improvement Medical Record
- Page 65 and 66:
Quality Improvement Institute for C
- Page 67 and 68:
Quality Improvement Quality Improve
- Page 69 and 70:
Quality Improvement Physical Facili
- Page 71 and 72:
Quality Improvement Treatment Recor
- Page 73 and 74:
Quality Improvement Treatment Recor
- Page 75 and 76:
Quality Improvement Treatment Recor
- Page 77 and 78:
Integrated Health Management Progra
- Page 79 and 80:
Integrated Health Management Provid
- Page 81 and 82:
Integrated Health Management Utiliz
- Page 83 and 84:
Integrated Health Management Medica
- Page 85 and 86:
Integrated Health Management Medica
- Page 87 and 88:
Integrated Health Management Overvi
- Page 89 and 90:
Integrated Health Management Pre-Ce
- Page 91 and 92:
Integrated Health Management Decisi
- Page 93 and 94:
Integrated Health Management Defini
- Page 95 and 96:
Integrated Health Management For Lo
- Page 97 and 98:
Integrated Health Management Appeal
- Page 99 and 100:
Integrated Health Management Case &
- Page 101 and 102:
Integrated Health Management Diseas
- Page 103 and 104:
Integrated Health Management Focuse
- Page 105 and 106:
Integrated Health Management Specia
- Page 107 and 108:
Integrated Health Management Overvi
- Page 109 and 110:
Integrated Health Management Medica
- Page 111 and 112:
Integrated Health Management Sample
- Page 113 and 114:
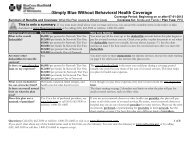
Health Care Options Prepaid Medical
- Page 115 and 116:
Health Care Options Member ID Cards
- Page 117 and 118:
Health Care Options Blue Cross and
- Page 119 and 120:
Health Care Options Double Gold Dou
- Page 121 and 122:
Health Care Options Medicare Basic
- Page 123 and 124:
Health Care Options Platinum Blue S
- Page 125 and 126:
Health Care Options MedicareBlue PP
- Page 127 and 128:
Health Care Options Inquiries and C
- Page 129 and 130:
Health Care Options Additional info
- Page 131 and 132:
Health Care Options Minnesota Senio
- Page 133 and 134:
Health Care Options MinnesotaCare P
- Page 135 and 136:
Health Care Options BlueLinkTPA Blu
- Page 137 and 138:
Health Care Options Delta Dental Hi
- Page 139 and 140:
Health Care Options Prime Therapeut
- Page 141 and 142:
Health Care Options Workers' Compen
- Page 143 and 144:
Health Care Options HICF 1500 Form
- Page 145 and 146:
Health Care Options Networks Blue C
- Page 147 and 148:
Blue Plus Member Information Introd
- Page 149 and 150:
Blue Plus Member Rights and Respons
- Page 151 and 152:
Blue Plus Member Rights and Respons
- Page 153 and 154:
Blue Plus Member Benefits Members
- Page 155 and 156:
Blue Plus Quality of Care Complaint
- Page 157 and 158:
Blue Plus Referral Points Remember
- Page 159 and 160:
Blue Plus Referral Not Required We
- Page 161 and 162:
Blue Plus Standing Referral Minneso
- Page 163 and 164:
Blue Plus Clarifications of Terms (
- Page 165 and 166:
Blue Plus [Date] [Name of patient]
- Page 167 and 168:
Blue Plus Special Member Benefits O
- Page 169 and 170:
Blue Plus OB/GYN Open Access Diagno
- Page 171 and 172:
Blue Plus OB/GYN Open Access Diagno
- Page 173 and 174:
BlueCard® Claim Status Inquiry ...
- Page 175 and 176:
BlueCard® Identifying BlueCard ®
- Page 177 and 178:
BlueCard® Identifying BlueCard ®
- Page 179 and 180:
BlueCard® BlueCard Service Claims
- Page 181 and 182:
BlueCard® Prior Authorization and
- Page 183 and 184:
BlueCard® Electronic Data Intercha
- Page 185 and 186:
BlueCard® Claims Processed by the
- Page 187 and 188:
BlueCard® Overview (continued) 3.
- Page 189 and 190:
BlueCard® Claim Payment Guidelines
- Page 191 and 192:
BlueCard® Calls from Members and O
- Page 193 and 194:
BlueCard® Guidelines (continued) W
- Page 195 and 196:
BlueCard® Types of Medicare Advant
- Page 197 and 198:
BlueCard® Medicare Advantage Claim
- Page 199 and 200:
BlueCard® Reimbursement for Medica
- Page 201 and 202:
Claims Filing HCPCS/ Accommodation
- Page 203 and 204:
Claims Filing Administrative Simpli
- Page 205 and 206:
Claims Filing Claims with Attachmen
- Page 207 and 208:
Claims Filing Claims with Coordinat
- Page 209 and 210:
Claims Filing Claims with Coordinat
- Page 211 and 212:
Claims Filing 1500 HICF Form Profes
- Page 213 and 214:
Claims Filing Ordering Forms and Ma
- Page 215 and 216:
Claims Filing Site of Service (cont
- Page 217 and 218:
Claims Filing Institution (837I) /F
- Page 219 and 220:
Claims Filing Treatment Room Blue C
- Page 221 and 222:
Claims Filing Single facility claim
- Page 223 and 224:
Claims Filing Present on Admission
- Page 225 and 226:
Claims Filing Medicare Crossover Bl
- Page 227 and 228:
Claims Filing Cancel/Void and Repla
- Page 229 and 230:
Claims Filing Cancel/Void and Repla
- Page 231 and 232:
Claims Filing Cancel/Void and Repla
- Page 233 and 234:
Claims Filing Verifying Patient Eli
- Page 235 and 236:
Claims Filing Basic Character Set V
- Page 237 and 238:
Claims Filing Rural Health Clinics
- Page 239 and 240:
Claims Filing Coordination of Benef
- Page 241 and 242:
Claims Filing TEFRA The 1982 Tax Eq
- Page 243 and 244:
Claims Filing Employment As defined
- Page 245 and 246:
Claims Filing Surgical Technicians
- Page 247 and 248:
Reimbursement / Reconciliation Reim
- Page 249 and 250:
Reimbursement / Reconciliation Comp
- Page 251 and 252:
Reimbursement / Reconciliation Remi
- Page 253 and 254:
Reimbursement / Reconciliation Ques
- Page 255 and 256:
Reimbursement / Reconciliation Ques
- Page 257 and 258:
Reimbursement / Reconciliation Acco
- Page 259 and 260:
Reimbursement / Reconciliation Fiel
- Page 261 and 262:
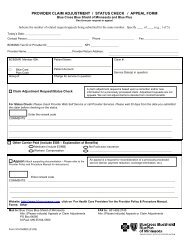
Appeals Provider Appeals Introducti
- Page 263 and 264:
Appeals Submitting Requests for Pos
- Page 265 and 266:
Appeals Coding Appeals (continued)
- Page 267 and 268:
Appeals Supporting Documentation (c
- Page 269 and 270:
Coding Policies and Guidelines (Cod
- Page 271 and 272:
Coding Policies and Guidelines (Cod
- Page 273 and 274:
Coding Policies and Guidelines (Cod
- Page 275 and 276:
Coding Policies and Guidelines (Cod
- Page 277 and 278:
Coding Policies and Guidelines (Cod
- Page 279 and 280:
Coding Policies and Guidelines (Cod
- Page 281 and 282:
Coding Policies and Guidelines (Cod
- Page 283 and 284:
Coding Policies and Guidelines (Cod
- Page 285 and 286:
Coding Policies and Guidelines (Cod
- Page 287 and 288:
Coding Policies and Guidelines (Cod
- Page 289 and 290:
Coding Policies and Guidelines (Cod
- Page 291 and 292:
Coding Policies and Guidelines (Cod
- Page 293 and 294:
Coding Policies and Guidelines (Cod
- Page 295 and 296:
Coding Policies and Guidelines (Cod
- Page 297 and 298:
Coding Policies and Guidelines (Cod
- Page 299 and 300:
Coding Policies and Guidelines (Cod
- Page 301 and 302:
Coding Policies and Guidelines (Cop
- Page 303 and 304:
Coding Policies and Guidelines (Mod
- Page 305 and 306:
Coding Policies and Guidelines (Mod
- Page 307 and 308:
Coding Policies and Guidelines (Mod
- Page 309 and 310:
Coding Policies and Guidelines (Mod
- Page 311 and 312:
Coding Policies and Guidelines (Mod
- Page 313 and 314:
Coding Policies and Guidelines (Mod
- Page 315 and 316:
Coding Policies and Guidelines (Mod
- Page 317 and 318:
Coding Policies and Guidelines (Mod
- Page 319 and 320:
Coding Policies and Guidelines (Mod
- Page 321 and 322:
Coding Policies and Guidelines (Mod
- Page 323 and 324:
Coding Policies and Guidelines (Mod
- Page 325 and 326:
Chapter 11 Coding Policies and Guid
- Page 327 and 328:
Part-time (Medically Directed) Anes
- Page 329 and 330:
Electroconvulsive Treatments Blue C
- Page 331 and 332:
Moderate (Conscious) Sedation Monit
- Page 333 and 334:
Chapter 11 Coding Policies and Guid
- Page 335 and 336:
Coding Policies and Guidelines (Beh
- Page 337 and 338:
Coding Restrictions Code Restrictio
- Page 339 and 340:
CTSS Skills Training and Developmen
- Page 341 and 342:
Intensive Residential Treatment Ser
- Page 343 and 344:
IRTS Member Eligibility IRTS Access
- Page 345 and 346:
Adult Non-Residential Crisis Servic
- Page 347 and 348:
MH-TCM Services to Minnesota Health
- Page 349 and 350:
Dialectical Behavioral Therapy/DBT
- Page 351 and 352:
Autism Spectrum Disorder/EIBI (cont
- Page 353 and 354:
Autism Spectrum Disorder/EIBI (cont
- Page 355 and 356:
Psychiatric Consultation to Primary
- Page 357 and 358:
Psychiatry and Chemical Dependency
- Page 359 and 360:
Medication Management M0064 and 908
- Page 361 and 362:
Nutritional Counseling/Medical Nutr
- Page 363 and 364:
Coding Policies and Guidelines (Beh
- Page 365 and 366:
Coding Policies and Guidelines (Beh
- Page 367 and 368:
Coding Policies and Guidelines (Beh
- Page 369 and 370:
Practitioner Key MD = Psychiatrist
- Page 371 and 372:
Clinical Supervision Under Minnesot
- Page 373 and 374:
DIAMOND Initiative (continued) Reim
- Page 375 and 376:
Coding Policies and Guidelines (Beh
- Page 377 and 378:
Missed Appointments (continued) Cou
- Page 379 and 380:
Guidelines for Court Ordered Evalua
- Page 381 and 382:
Guidelines for Court Ordered Evalua
- Page 383 and 384:
Coding Policies and Guidelines (Beh
- Page 385 and 386:
Behavioral Health Quality Improveme
- Page 387 and 388:
Pre-certification and Concurrent Re
- Page 389:
Coding Policies and Guidelines (Beh
- Page 392 and 393:
Coding Policies and Guidelines (Beh
- Page 394 and 395:
Coding Policies and Guidelines (Beh
- Page 396 and 397:
Coding Policies and Guidelines (Beh
- Page 398 and 399:
Coding Policies and Guidelines (Beh
- Page 400 and 401:
Coding Policies and Guidelines (Beh
- Page 402 and 403:
Coding Policies and Guidelines (Beh
- Page 404 and 405:
Coding Policies and Guidelines (Beh
- Page 406 and 407:
Coding Policies and Guidelines (Beh
- Page 408 and 409:
Coding Policies and Guidelines (Beh
- Page 410 and 411:
Coding Policies and Guidelines (Beh
- Page 412 and 413:
Coding Policies and Guidelines (Beh
- Page 414 and 415:
Coding Policies and Guidelines (Beh
- Page 416 and 417:
Coding Policies and Guidelines (Beh
- Page 418 and 419:
Coding Policies and Guidelines (Beh
- Page 420 and 421:
Coding Policies and Guidelines (Beh
- Page 422 and 423:
Coding Policies and Guidelines (Beh
- Page 424 and 425:
Coding Policies and Guidelines (Beh
- Page 426 and 427:
Coding Policies and Guidelines (Beh
- Page 428 and 429:
Coding Policies and Guidelines (Beh
- Page 430 and 431:
Coding Policies and Guidelines (Beh
- Page 432 and 433:
Coding Policies and Guidelines (Beh
- Page 434 and 435:
Coding Policies and Guidelines (Beh
- Page 436 and 437:
Coding Policies and Guidelines (Beh
- Page 438 and 439:
Coding Policies and Guidelines (Beh
- Page 440 and 441:
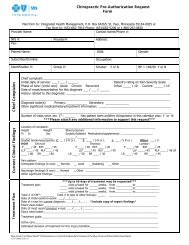
Coding Policies and Guidelines (Chi
- Page 442 and 443:
Coding Policies and Guidelines (Chi
- Page 444 and 445:
Coding Policies and Guidelines (Chi
- Page 446 and 447:
Coding Policies and Guidelines (Chi
- Page 448 and 449:
Coding Policies and Guidelines (Chi
- Page 450 and 451:
Coding Policies and Guidelines (Chi
- Page 452 and 453:
Coding Policies and Guidelines (Den
- Page 454 and 455:
Coding Policies and Guidelines (Den
- Page 456 and 457:
Chapter 11 Coding Policies and Guid
- Page 458 and 459:
Prior Authorization Requirements Co
- Page 460 and 461:
Coding Policies and Guidelines (Dur
- Page 462 and 463:
Waivers and Upgraded/Deluxe DME Wai
- Page 464 and 465:
Coding Policies and Guidelines (Dur
- Page 466 and 467:
Hearing Aids (continued) Website Co
- Page 468 and 469:
Portable Oxygen Billing (continued)
- Page 470 and 471:
Coding Policies and Guidelines (Dur
- Page 472 and 473:
DME/Supply Internet Purchases Codin
- Page 474 and 475:
Chapter 11 Coding Policies and Guid
- Page 476 and 477:
Coding Policies and Guidelines (Hom
- Page 478 and 479:
Elderly Waiver Program (continued)
- Page 480 and 481:
Referrals and Prior Authorization (
- Page 482 and 483:
Referrals and Prior Authorization (
- Page 484 and 485:
Adult Day Care Bath Services Coding
- Page 486 and 487:
Home Infusion (continued) Coding Po
- Page 488 and 489:
Coding Policies and Guidelines (Hom
- Page 490 and 491:
Rules and Regulations (continued) H
- Page 492 and 493:
Hospice Billing for Medicare Produc
- Page 494 and 495:
Coding Policies and Guidelines (Hos
- Page 496 and 497:
Coding Policies and Guidelines (Hos
- Page 498 and 499:
Coding Policies and Guidelines (Hos
- Page 500 and 501:
Coding Policies and Guidelines (Hos
- Page 502 and 503:
Chapter 11 Coding Policies and Guid
- Page 504 and 505:
Coding Policies and Guidelines (Lab
- Page 506 and 507:
Papanicolaou Smears (continued) Dia
- Page 508 and 509:
Blue Cross and Blue Shield of Minne
- Page 510 and 511:
Coding Policies and Guidelines (Mat
- Page 512 and 513:
Coding Policies and Guidelines (Mat
- Page 514 and 515:
Coding Policies and Guidelines (Mat
- Page 516 and 517:
Coding Policies and Guidelines (Mat
- Page 518 and 519:
Coding Policies and Guidelines (Mat
- Page 520 and 521:
Coding Policies and Guidelines (Med
- Page 522 and 523:
Coding Policies and Guidelines (Med
- Page 524 and 525:
Coding Policies and Guidelines (Med
- Page 526 and 527:
Coding Policies and Guidelines (Med
- Page 528 and 529:
Coding Policies and Guidelines (Med
- Page 530 and 531:
Coding Policies and Guidelines (Med
- Page 532 and 533:
Coding Policies and Guidelines (Med
- Page 534 and 535:
Coding Policies and Guidelines (Med
- Page 536 and 537:
Coding Policies and Guidelines (Med
- Page 538 and 539:
Coding Policies and Guidelines (Med
- Page 540 and 541:
Coding Policies and Guidelines (Med
- Page 542 and 543:
Coding Policies and Guidelines (Med
- Page 544 and 545:
Coding Policies and Guidelines (Med
- Page 546 and 547:
Coding Policies and Guidelines (Med
- Page 548 and 549:
Coding Policies and Guidelines (Med
- Page 550 and 551:
Coding Policies and Guidelines (Med
- Page 552 and 553:
Coding Policies and Guidelines (Med
- Page 554 and 555:
Coding Policies and Guidelines (Med
- Page 556 and 557:
Coding Policies and Guidelines (Med
- Page 558 and 559: Coding Policies and Guidelines (Med
- Page 560 and 561: Coding Policies and Guidelines (Med
- Page 562 and 563: Coding Policies and Guidelines (Med
- Page 564 and 565: Coding Policies and Guidelines (Med
- Page 566 and 567: Coding Policies and Guidelines (Med
- Page 568 and 569: Coding Policies and Guidelines (Med
- Page 570 and 571: Coding Policies and Guidelines (Med
- Page 572 and 573: Coding Policies and Guidelines (Med
- Page 574 and 575: Coding Policies and Guidelines (Med
- Page 576 and 577: Coding Policies and Guidelines (Med
- Page 578 and 579: Coding Policies and Guidelines (Med
- Page 580 and 581: Coding Policies and Guidelines (Opt
- Page 582 and 583: Chapter 11 Coding Policies and Guid
- Page 584 and 585: Coding Policies and Guidelines (Pha
- Page 586 and 587: Drugs Coding Policies and Guideline
- Page 588 and 589: Coding Policies and Guidelines (Pha
- Page 590 and 591: Drug Programs Coding Policies and G
- Page 592 and 593: Coding Policies and Guidelines (Pha
- Page 594 and 595: Coding Policies and Guidelines (Pub
- Page 596 and 597: Coding Policies and Guidelines (Pub
- Page 598 and 599: Coding Policies and Guidelines (Pub
- Page 600 and 601: Coding Policies and Guidelines (Pub
- Page 602 and 603: Coding Policies and Guidelines (Pub
- Page 604 and 605: Coding Policies and Guidelines (Pub
- Page 606 and 607: Coding Policies and Guidelines (Pub
- Page 610 and 611: Coding Policies and Guidelines (Pub
- Page 612 and 613: Coding Policies and Guidelines (Pub
- Page 614 and 615: Coding Policies and Guidelines (Pub
- Page 616 and 617: Coding Policies and Guidelines (Pub
- Page 618 and 619: Coding Policies and Guidelines (Pub
- Page 620 and 621: Coding Policies and Guidelines (Pub
- Page 622 and 623: Coding Policies and Guidelines (Pub
- Page 624 and 625: Coding Policies and Guidelines (Rad
- Page 626 and 627: Coding Policies and Guidelines (Rad
- Page 628 and 629: Coding Policies and Guidelines (Rad
- Page 630 and 631: Chapter 11 Coding Policies and Guid
- Page 632 and 633: Physical Therapy Evaluation Codes C
- Page 634 and 635: Hot and Cold Pack Exclusion TMJ Ort
- Page 636 and 637: Massage and Manual Therapy Exclusio
- Page 638 and 639: MHCP PT, OT, ST Authorization Proce
- Page 640 and 641: Chapter 11 Coding Policies and Guid
- Page 642 and 643: Bilateral Services (continued) Codi
- Page 644 and 645: Coding Policies and Guidelines (Sur
- Page 646 and 647: Acne Treatment/ Skin Rejuvenation a
- Page 648 and 649: Liposuction Edit Change Coding Poli
- Page 650 and 651: Assistant Surgeons (continued) Assi
- Page 652: Coding Policies and Guidelines (Sur