- Page 1 and 2:
A-PDF Merger DEMO : Purchase from w
- Page 3 and 4:
It contains : - 46 (23 pairs) of ch
- Page 5 and 6:
6. Glycolipids - signal molecules.
- Page 7 and 8:
Eukaryotic cell cycle : - Human bod
- Page 9 and 10:
• Regulation of the cell cycle :
- Page 11 and 12:
11
- Page 13 and 14:
• Morphology of apoptosis (EM) :
- Page 16 and 17:
Ion transport - Trans-membrane ion
- Page 18 and 19:
18
- Page 20 and 21:
20
- Page 22 and 23:
22
- Page 24:
Disease Signal transduction Ligands
- Page 27 and 28:
Example of GP-CR → Adrenergic rec
- Page 29 and 30:
29
- Page 31 and 32:
- There are around 30,000 gene , on
- Page 33 and 34:
- The language used by DNA is calle
- Page 35 and 36:
Autosomal dominant Autosomal recess
- Page 37 and 38:
Modes of disease inheritance Autos
- Page 39 and 40:
Autosomal dominant conditions Very
- Page 41 and 42:
X-linked dominant inheritance - The
- Page 43 and 44:
Fragile X syndrome : - Trinucleotid
- Page 45 and 46:
Some common genetic syndromes Triso
- Page 47 and 48:
Edwards Syndrome - Also known as Tr
- Page 49 and 50:
• Prognosis of Marfan syndrome -
- Page 51 and 52:
Noonan Syndrome - Often thought of
- Page 53 and 54:
Immune system - Immunity is the lin
- Page 55 and 56:
Classification of immunity Innate i
- Page 58:
Immune response to pathogen : A) In
- Page 61 and 62:
Expression Structure MHC I - In all
- Page 63 and 64:
C) Adaptive immune response : - The
- Page 65 and 66:
Cytokines produced by different kin
- Page 67 and 68:
ANCA o There are two main types of
- Page 69 and 70:
Tolerance & autoimmunity : o The im
- Page 71 and 72:
Complement system o It`s a group of
- Page 73 and 74:
Inflammation o Inflammation is a no
- Page 75 and 76:
o Immunosuppressive therapy is used
- Page 77 and 78:
C. Antimetabolites Cytotoxic Mechan
- Page 79 and 80:
o The mode of action of sirolimus i
- Page 81 and 82:
Primary immunodeficiency o Primary
- Page 83 and 84:
o Recently, a further category has
- Page 85 and 86:
- Reabsorption of HCO3 - (85% in PC
- Page 87 and 88:
Pathogenesis: Causes : Features : T
- Page 89 and 90:
A) Respiratory centers depression A
- Page 91 and 92:
o Treatment of chronic respiratory
- Page 93 and 94:
Saline - Responsive metabolic alkal
- Page 95 and 96:
Hypertonic Isotonic Hypotonic Plasm
- Page 97 and 98:
Hypernatremia (Na + > 145 mmol/L) :
- Page 99 and 100:
Hyperkalemia (K + > 5.2 mmo/L) : -
- Page 101 and 102:
Hypokalemia - Potassium and hydroge
- Page 103 and 104:
Medical statistics • Def : • St
- Page 105 and 106:
MEDIAN (=mid-point) Def : It is the
- Page 107 and 108:
Q : A study is performed to find th
- Page 109 and 110:
- Whilst correlation coefficients g
- Page 111 and 112:
Statistics which test differences P
- Page 113 and 114:
B. Statistics which test confidence
- Page 115 and 116:
P- VALUES • Def : - The P (propab
- Page 117 and 118:
Q 1: Q2 : If a drug reduces the inc
- Page 119 and 120:
Q4 : - CER (Aspirin) = 3% - EER (ne
- Page 121 and 122:
SPECIFICITY = →This is the rate a
- Page 123 and 124:
Q : 123
- Page 125 and 126:
Randomised controlled trial Experim
- Page 127 and 128:
Case-control study • Def : - It`s
- Page 129 and 130:
Study Design: Evidence and Recommen
- Page 131 and 132:
Intention to treat analysis Q - It
- Page 133 and 134:
CORONARY ARTERY DISEASES Definitio
- Page 135 and 136:
Risk factors of CAD: High risk fac
- Page 137 and 138:
Stable (chronic) angina (= angina o
- Page 139 and 140:
A) Medical ttt of stable angina(CKS
- Page 141 and 142:
DVLA rules: cardiovascular disorder
- Page 143 and 144:
STMI NSTMI/UA ACS < 12 hrs of symto
- Page 145 and 146:
• Treatment : A. Medical TTT : I
- Page 147 and 148:
Cardiac arrhythmias I. Tachyarrhyth
- Page 149 and 150:
Atrial fibrillation (AF) Def : - o
- Page 151 and 152:
2. Echocardiography: - Significant
- Page 153 and 154:
Acute newly detected AF Hemodynamic
- Page 155 and 156:
Rate vs rhythm control : Factors fa
- Page 157 and 158:
Digoxin and digoxin toxicity - Digo
- Page 159 and 160:
Long QT syndrome Def: - Long QT syn
- Page 161 and 162:
Conducting system of the heart : He
- Page 163 and 164:
Ventricular tachycardia Ventricular
- Page 165 and 166:
• Treatment of shockable rhythms
- Page 167 and 168:
Peri-arrest rhythms A. Peri-arrest
- Page 169 and 170:
B. Peri-arrest tachycardia Hemodyna
- Page 171 and 172:
QRS Deflection Inferior leads (II,I
- Page 173 and 174:
B-type natriuretic peptide (BNP) :
- Page 175 and 176:
Hypertension Clinic BP measurement
- Page 177 and 178:
Stepwise approach of treatment of H
- Page 179 and 180:
Pulmonary arterial hypertension(PAH
- Page 181 and 182:
Normal pulse in young (25y) person
- Page 183 and 184:
Jugular venous pulse(JVP) 52
- Page 185 and 186:
Valvular heart disease Aortic steno
- Page 187 and 188:
• Features Aortic regurgitation
- Page 189 and 190:
• Echocardiography : A 'tight' m
- Page 191 and 192:
Murmur Causes Character Point of ma
- Page 193 and 194:
Pericarditis Pericarditis is one of
- Page 195 and 196:
Myocarditis • Causes Viral: Coxs
- Page 197 and 198:
- Most of cardiologists proceeds to
- Page 199 and 200:
Causes of sudden cardiac death : In
- Page 201 and 202:
2) Atrial Septal Defects (ASDs) - T
- Page 203 and 204:
Eisenmenger's syndrome - In acyanot
- Page 205 and 206:
- When properly positioned, the dis
- Page 207 and 208:
Down syndrome - Down syndrome is th
- Page 209 and 210:
Marfan's syndrome - Marfan's syndro
- Page 211 and 212:
Causes: - Streptococcus viridans (m
- Page 213 and 214:
Treatment of IE : A) Medical ttt :
- Page 215 and 216:
CVS medications Antiarrhythmic drug
- Page 217 and 218:
Amiodarone Class : III antiarrhyth
- Page 219 and 220:
‣ Β- blockers cardiotoxicity : -
- Page 221 and 222:
Aspirin : Mechanism of action : -
- Page 223 and 224:
Diuretics : Thiazides Diuretics Act
- Page 225 and 226:
lesions Macule Patch Papule Nodule
- Page 227 and 228:
Acne vulgaris - Acne vulgaris is a
- Page 229 and 230:
Isotretinoin - Is an oral retinoid
- Page 231 and 232:
Pityriasis Versicolor (= tinea vers
- Page 233 and 234:
Plaque psoriasis Flexural psoriasis
- Page 235 and 236:
- Finger tip rule 1 finger tip uni
- Page 237 and 238:
D. Contact dermatitis - Contact der
- Page 239 and 240:
Pemphigus vulgaris - Is an autoimmu
- Page 241 and 242:
Erythematous skin rash Erythema mul
- Page 243 and 244:
Erythema nodosum - Idiopathic condi
- Page 245 and 246:
Lichen-like diseases - Lichens are
- Page 247 and 248:
Scabies • Overview : - It is a pr
- Page 249 and 250:
Diseases of hairs Hirsuitism & Hype
- Page 251 and 252:
Diseases of the nails Onycholysis -
- Page 253 and 254:
Skin infections Impetigo - Is a hig
- Page 255 and 256:
Pyoderma Gangrenosum - Is a conditi
- Page 257 and 258:
Granuloma annulare - Papular lesion
- Page 259 and 260:
Molluscum contagiosum - Flesh-white
- Page 261 and 262:
Skin disorders associated with mali
- Page 263 and 264:
*Langer lines were historically use
- Page 266 and 267:
Pituitary gland Anatomy : - Small
- Page 268 and 269:
Diseases of pituitary gland Anterio
- Page 270 and 271:
Anterior pituitary hpofunction in a
- Page 272 and 273:
Anterior pituitary hyperfunction I.
- Page 274 and 275:
o Hands & feet : - Spade-like hands
- Page 276 and 277:
Prolactin is unique amongst the pit
- Page 278 and 279:
Very rare drug causes of gynaecomas
- Page 280 and 281:
Investigations : 1) High plasma osm
- Page 282 and 283:
Treatment of DI : Cranial DI (ie wi
- Page 284 and 285:
Non-functioning adenoma (chromophob
- Page 286 and 287:
Thyroid gland Anatomy : - Butterfl
- Page 288 and 289:
Control of thyroid hormones (hypoth
- Page 290 and 291:
o Thyrotoxic crisis (thyroid storm)
- Page 292 and 293:
- Graves' disease is the most commo
- Page 294 and 295:
Subclinical Hyperthyroidism - It is
- Page 296 and 297:
Myxoedema Causes : Primary hypothy
- Page 298 and 299:
Subclinical Hypothyroidism Basics
- Page 300 and 301:
Thyroiditis - i.e Inflammation of t
- Page 302 and 303:
- It`s the commonest endocrine mali
- Page 305:
Amiodarone-induced thyroid disease
- Page 308 and 309:
Actions of parathyroid hormone ( pl
- Page 310 and 311:
Latent tetany +ve Provocative tests
- Page 312 and 313:
■ Clinical picture : Bones, Stone
- Page 314 and 315:
Hyperparathyroidism - i.e over prod
- Page 316 and 317:
Hypoparathyroidism - i.e decrease p
- Page 318 and 319:
- Histologically : bone is formed o
- Page 320 and 321:
• Management : (NICE 2011 ,2ndry
- Page 322 and 323:
8) Hip protectors : - Evidence to s
- Page 324 and 325:
Osteomalacia Def : - Defective min
- Page 326 and 327:
Osteogenesis Imperfecta (= brittle
- Page 328 and 329:
• Functions of adrenal hormones :
- Page 330 and 331:
Primary hyperaldosteronism Causes
- Page 332 and 333:
Investigations : A. Diagnosis of Cu
- Page 334 and 335:
Adrenal insufficiency Causes : o P
- Page 336 and 337:
Differences between 1ry & 2ndry adr
- Page 338 and 339:
Def : Diabetes Mellitus (DM) - Met
- Page 340 and 341:
سؤال اليخلو منه امت
- Page 343 and 344:
3)Other risk factor modification C
- Page 345 and 346:
I. Insulin sensitizers 1) Biguanide
- Page 347 and 348:
■ Management of type I DM [Insuli
- Page 349 and 350:
5) Insulin resistance (i.e requirem
- Page 351 and 352:
Complications of DM : Complication
- Page 353 and 354:
Diabetic foot ulcers : • Classifi
- Page 355 and 356:
Investigations : سؤال amylase.
- Page 357 and 358:
Treatment of HONK : as in DKA with
- Page 359 and 360:
D. Post delivery : DC TTT(in GDM) ,
- Page 361 and 362:
Insulinoma is a neuroendocrine tumo
- Page 363 and 364:
Def : body mass index ( BMI) > 30 O
- Page 365 and 366:
■ Sibutramine - Withdrawn January
- Page 367 and 368:
- Dietary fat (TG) is digested by b
- Page 369 and 370:
Classification of hyperlipidemia :
- Page 371 and 372:
• Management Referral to a speci
- Page 373 and 374:
• Physiology of reproductive syst
- Page 375 and 376:
• Def : Delayed growth & puberty
- Page 377 and 378:
Hypogonadism ■ Def: - A diminishe
- Page 379 and 380:
MRI →Absence of olfactory bulb.
- Page 381 and 382:
• Initial investigations Exclude
- Page 383 and 384:
■ Diagnostic approach of 2ndry am
- Page 385 and 386:
تبدو وتتصرف ك بنت و
- Page 387 and 388:
■ Diagnosis : ■ Treatment : Kar
- Page 389 and 390:
3) Infertility : (under specialist
- Page 391 and 392:
Carcinoid tumours - Group of slowly
- Page 393 and 394:
1
- Page 395 and 396:
• Hormones of GIT : Hormone Gastr
- Page 397 and 398:
• Treatment : A. Acute treatment
- Page 399 and 400:
• DD (causes of heart burn sensat
- Page 401 and 402:
Dysphagia - The table below gives c
- Page 403 and 404:
Disease Achalasia Scleroderma Manom
- Page 405 and 406:
Oesophageal cancer - The most commo
- Page 407 and 408:
سؤال مهم : dyspepsia Drug-in
- Page 409 and 410:
Management of endoscopy proven gast
- Page 411 and 412:
Management of endoscopy proven non-
- Page 413 and 414:
• Investigations of H.Pylori : س
- Page 415 and 416:
• Clinical features of ZES : Zoll
- Page 417 and 418:
• Diagnosis: • Staging : Endosc
- Page 419 and 420:
Coeliac disease • Def : - An auto
- Page 421 and 422:
B. Jejunal biopsy (see pathology).
- Page 423 and 424:
• Investigations : 1) Jejuna biop
- Page 425 and 426:
Short bowel syndrome - Malabsorptio
- Page 427 and 428:
Inherited (familial) colorectal can
- Page 429 and 430:
Pelvi-abdominal CT/MRI/PET scan wit
- Page 431 and 432:
Acute Intestinal ischemia • Def :
- Page 433 and 434:
سؤال امتحان Melanosis col
- Page 435 and 436:
Inflammatory bowel diseases (IBD)
- Page 437 and 438:
Histology Involve whole bowel wall
- Page 439 and 440:
B. Management of ulcerative colitis
- Page 441 and 442:
هام : UC) Colo-rectal cancer on
- Page 443 and 444:
Acute infective diarrhea (infective
- Page 445 and 446:
• Management : 1) Rest ,rehydrati
- Page 447 and 448:
Liver diseases Hepatitis • Def :
- Page 449 and 450:
• Complications: Hepatitis C : 80
- Page 451 and 452:
Viral hepatitis B - HBV is a double
- Page 453 and 454:
• Immunisation (vaccination) agai
- Page 455 and 456:
• Risk factors of ALD : - Men : w
- Page 457 and 458:
Fatty liver (steatosis) - It`s live
- Page 459 and 460:
• Types according to the types of
- Page 461 and 462:
liver: hepatitis, cirrhosis lentif
- Page 463 and 464:
• Features Homozygous PiZZ →(A
- Page 465 and 466:
• Complications Malabsorption: o
- Page 467 and 468:
Chronic liver disease (cirrhosis)
- Page 469 and 470:
سؤال امتحان classificatio
- Page 471 and 472:
Meigs' Syndrome : = Ovarian fibroma
- Page 473 and 474:
Type I HRS Rapidly progressive. D
- Page 475 and 476:
Hepatic Encephalopathy: • Def: A
- Page 477 and 478:
Haemochromatosis: - Is an autosomal
- Page 479 and 480:
Hepatomegaly : • Common causes of
- Page 481 and 482:
B. Causes of conjugated (direct) hy
- Page 483 and 484:
Crigler-Najjar Syndrome (CNS): - (C
- Page 485 and 486:
Diseases of pancreas Acute pancreat
- Page 487 and 488:
Chronic Pancreatitis - Is an inflam
- Page 489 and 490:
• Diagnosis: Contrast CT is used
- Page 491 and 492:
Liver biopsy • Contraindications
- Page 493 and 494:
Diseases of RBCs Include 3 main gro
- Page 495 and 496:
Microcytic hypochromic anemias I. I
- Page 497 and 498:
II.Thalassemia - It`s an inherited
- Page 499 and 500:
• Pathogenesis of thalassemia : -
- Page 501 and 502:
Hb electrophoresis : - The major Hb
- Page 503 and 504:
• Management : 1) Phlebotomy (ven
- Page 505 and 506:
Chronic Hemolytic Anemia with acute
- Page 507 and 508:
Autoimmune hemolytic anemia (AIHA)
- Page 509 and 510:
- Hemolysis which ↑↑ during sle
- Page 511 and 512: • Causes: 1. Post-infection e.g.
- Page 513 and 514: Glucose-6-phosphate dehydrogenase (
- Page 515 and 516: - These other forms of sickle-cell
- Page 517 and 518: • Investigations : CBC : normocy
- Page 519 and 520: • WHO 2008 classification of MDS
- Page 521 and 522: Macrocytic megaloblastic anemias Ca
- Page 523 and 524: • Incidence - Peaks in the sixth
- Page 525 and 526: Hemoglobinopathies Quantitative (Im
- Page 527 and 528: • Typical carboxyhemoglobin level
- Page 529 and 530: Leukemoid reaction - Describes the
- Page 531 and 532: Hyper Eesinophilic syndrome: - Rare
- Page 533 and 534: B. Lympho-proliferative disorders (
- Page 535 and 536: - Further classification of each ty
- Page 537 and 538: • Management of AML : Chemothera
- Page 539 and 540: Chronic Myeloid Leukemia (CML) - Th
- Page 541 and 542: Chronic Lymphocytic Leukemia (CLL)
- Page 543 and 544: Incdence Commonest acute leukemia
- Page 545 and 546: • Ann-Arbor staging of Hodgkin's
- Page 547 and 548: - Chemotherapy includes : 1. Doxoru
- Page 549 and 550: Burkitt's Lymphoma : - Is a high-gr
- Page 551 and 552: Multiple myeloma - It`s a neoplasm
- Page 553 and 554: Diseases of platelets 1. Thrombocyt
- Page 555 and 556: • Causes of severe thrombocytopen
- Page 557 and 558: • Normal response to vessel injur
- Page 559 and 560: Von Willebrand's disease - Von Will
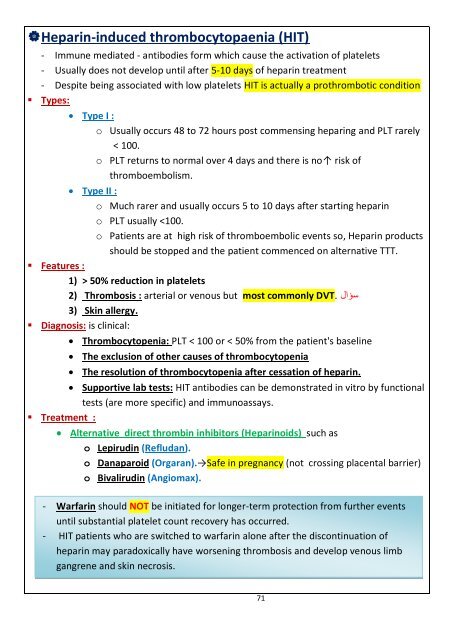
- Page 561: - There are two main types of hepar
- Page 565 and 566: 74
- Page 567 and 568: Acquired Factor VIII Deficiency - I
- Page 569 and 570: Thrombophilia ( = thrombotic tenden
- Page 571 and 572: Hyposplenism e.g. post-splenectomy
- Page 573 and 574: Graft versus host disease (GVHD) :
- Page 575 and 576: Tumour markers • Tumour markers m
- Page 577 and 578: C. Antimetabolites Cytotoxic Mechan
- Page 579 and 580: Therapeutic antibodies : Monoclonal
- Page 581 and 582: • Conversion between opioids From
- Page 583 and 584: Thymoma - Thymomas are the most com
- Page 585 and 586: Prostate cancer - Prostate cancer i
- Page 587 and 588: Oncogenes • Def : - They are endo
- Page 589 and 590: Classification of pathogens الح
- Page 591 and 592: Anaerobes Aerobes G-ve bacteria G-v
- Page 593 and 594: B. Whole killed organism (= inactiv
- Page 595 and 596: Necrotizing fasciitis : - Is a medi
- Page 597 and 598: A. Actinomycosis - Actynomyces is f
- Page 599 and 600: Clostridium difficile: - Is a Gram
- Page 601 and 602: 1. Septic arthritis ( the most comm
- Page 603 and 604: Atypical bacteria I. Mycobacterium
- Page 605 and 606: Extra-pulmonary TB ( in immunocompr
- Page 607 and 608: هام جدا : TB Management of Ac
- Page 609 and 610: III. Spirockaetes A. Leptospirosis
- Page 611 and 612: IV. Ricketsiae A. African Tick Typh
- Page 613 and 614:
• Management : A. Uncomplicated f
- Page 615 and 616:
- It is again advisable to avoid tr
- Page 617 and 618:
• Diagnosis : Splenic or bone ma
- Page 619 and 620:
• Investigation Antibody test S
- Page 621 and 622:
Cryptosporidium : سؤال - It`s t
- Page 623 and 624:
Antiretroviral group NRTI Examples
- Page 625 and 626:
B. Focal neurological lesions : 1)
- Page 627 and 628:
• Complications : A. Common compl
- Page 629 and 630:
• Complications : 1) Encephalitis
- Page 631 and 632:
6) Infectious mononucleosis (glandu
- Page 633 and 634:
8) Novel Coronavirus - Human corona
- Page 635 and 636:
B. Trematodes (flat worms) Schistos
- Page 637 and 638:
• Management (SIGN 2009) : Azyth
- Page 639 and 640:
Genital ulcers : Common causes of g
- Page 641 and 642:
Lymphogranuloma venereum سؤال t
- Page 643 and 644:
Mechanism of action of common antib
- Page 645 and 646:
Leprosy liptospirosis Lyme disease
- Page 647 and 648:
(Human papilloma virus) UTI in woma
- Page 649 and 650:
Osteomyelitis : - Osteomyelitis des
- Page 651 and 652:
مرض األغنام Orf - Orf is
- Page 653 and 654:
1
- Page 655 and 656:
3
- Page 657 and 658:
Diseases of thick ascending limb of
- Page 659 and 660:
III. According to clinical presenta
- Page 661 and 662:
9
- Page 663 and 664:
Minimal Change disease (MCD) - Near
- Page 665 and 666:
Management Minimal change glomerulo
- Page 667 and 668:
Focal Segmental Glomerulosclerosis
- Page 669 and 670:
B. I.F : no immune deposits (C3 & I
- Page 671 and 672:
3 rd line ttt Plasma exchange: - Th
- Page 673 and 674:
Causes : 1ry ( idiopathic) MCGN .
- Page 675 and 676:
New classification (according to th
- Page 677 and 678:
2) Type II MCGN : 25
- Page 679 and 680:
Membranous nephropathy (MN) - It`s
- Page 681 and 682:
Approaching MN : - Careful history
- Page 683 and 684:
Prognosis : (rule of thirds) 1/3 o
- Page 685 and 686:
IgA nephropathy Basics: Also calle
- Page 687 and 688:
Management of IgA nephropathy Low r
- Page 689 and 690:
Renal parenchymatous diseases accor
- Page 691 and 692:
NB : The antigens against which th
- Page 693 and 694:
Management of nephritic syndrome :
- Page 695 and 696:
Management: ACE-I ARBs Approximat
- Page 697 and 698:
Acute renal failure (now termed acu
- Page 699 and 700:
Causes of CKD : Common causes of CK
- Page 701 and 702:
Anemia in CRF: All types of anemia
- Page 703 and 704:
There is transformation among the p
- Page 705 and 706:
III. Pauci-immune (ANCA+ve) nephrop
- Page 707 and 708:
Hereditary renal disease I. Alport
- Page 709 and 710:
NEUROLOGY DR. MEDHAT M.SLEAT 2013
- Page 711 and 712:
Brain anatomy - It`s a gelatinous o
- Page 713 and 714:
C. Cerebellum : o It lies behind th
- Page 715 and 716:
Frontal lobe Area Site Function Les
- Page 717 and 718:
Parietal lobe Cortical sensory area
- Page 719 and 720:
Occipital lobe Visual sensory area
- Page 721 and 722:
Upper & lower motor neurons - For a
- Page 723 and 724:
U.M.N. Lesion L.M.N. Lesion Paralys
- Page 725 and 726:
اللهم السهل اال ماج
- Page 727 and 728:
II. Optic nerve • Pathway of visi
- Page 729 and 730:
III. Oculomotor nerve - The nucleus
- Page 731 and 732:
IV. Trochlear nerve : - The nucleus
- Page 733 and 734:
V. Trigeminal nerve : - It`s a mixe
- Page 735 and 736:
• Trigeminal nerve palsy: o Cause
- Page 737 and 738:
سؤال هام فى اال متح
- Page 739 and 740:
VII.Facial nerve : - it`s a mixed n
- Page 741 and 742:
U.M.N.L Affects ∆ tract above fac
- Page 743 and 744:
VI. Vestibule-cochlear nerve : - Th
- Page 745 and 746:
VII. Glossopharyngeal nerve : - It`
- Page 747 and 748:
Petrous apex syndrome : • Causes
- Page 749 and 750:
Control of eye movement during head
- Page 751 and 752:
Conjugate gaze palsy Supranuclear N
- Page 753 and 754:
Carotid (anterior) system : Anterio
- Page 755 and 756:
47
- Page 757 and 758:
Basilar artery • Origin : - Forme
- Page 759 and 760:
B. Total occlusion : is fatal 1. De
- Page 761 and 762:
Middle cerebral artery Anterior cer
- Page 763 and 764:
Posterior inferior cerebellar arter
- Page 765 and 766:
IV. Carotid artery endarterectomy
- Page 767 and 768:
Subarachnoid hge (rupture aneurysm)
- Page 769 and 770:
• Clinical presentation : - Typic
- Page 771 and 772:
Traumatic brain injury: Extradural
- Page 773 and 774:
Medial pontine syndrome - e.g occlu
- Page 775 and 776:
• Prognosis : - Variable prognosi
- Page 777 and 778:
Incomplete lesions of spinal cord B
- Page 779 and 780:
Investigations 1. Decreased red cel
- Page 781 and 782:
• Management In primary care; a
- Page 783 and 784:
Lewy body dementia - Is the second
- Page 785 and 786:
Transient global amnesia (TGA) •
- Page 787 and 788:
• Management : Riluzole 1. Anti-
- Page 789 and 790:
Gower`s sign of Duchenne`s muscle d
- Page 791 and 792:
• Management : - 1 st line invest
- Page 793 and 794:
Pricipitating factors of myasthenia
- Page 795 and 796:
- *In reality this is seen in only
- Page 797 and 798:
- The basal ganglia and cerebellum
- Page 799 and 800:
• Extra pyramidal tracts : Tract
- Page 801 and 802:
• Main clinical features : Dyskin
- Page 803 and 804:
2) Levodopa: Usually combined with
- Page 805 and 806:
III. Hemiballism (subthalamus) - Oc
- Page 807 and 808:
• Investigation of choice : MRI (
- Page 809 and 810:
Cerebellar syndromes : Archicerebe
- Page 811 and 812:
Herido-familaial ataxia : A. Friedr
- Page 813 and 814:
سؤال امتحان Meniere's dis
- Page 815 and 816:
Nystagmus - Oscillatory eye movemen
- Page 817 and 818:
Diseases of the nerves • Def : -
- Page 819 and 820:
2. Predominantly sensory : o Friedr
- Page 821 and 822:
Common peroneal nerve (L4,5 & S1,2)
- Page 823 and 824:
Femoral nerve o Origin : lumbar ple
- Page 825 and 826:
L3 nerve root compression L4 nerve
- Page 827 and 828:
Nerve supply of the upper limb Medi
- Page 829 and 830:
121
- Page 831 and 832:
Carpal tunnel syndrome • Def : Mo
- Page 833 and 834:
Sensory to : 1. Dorsal aspect of la
- Page 835 and 836:
Elbow Pain: - The table below detai
- Page 837 and 838:
Reflex Biceps reflex Triceps reflex
- Page 839 and 840:
131
- Page 841 and 842:
Gastroparesis Symptoms include err
- Page 843 and 844:
Nerve Conduction Studies (NCS) - Ar
- Page 845 and 846:
- Complex partial seizures can take
- Page 847 and 848:
8. It is advised that pregnant wome
- Page 849 and 850:
سؤال امتحان : Cataplexy
- Page 851 and 852:
• Management : o Aim: reducing th
- Page 853 and 854:
Tuberous sclerosis (TS) - Autosomal
- Page 855 and 856:
• General C/P : ( it`s not a must
- Page 857 and 858:
Headache - Headache is the term use
- Page 859 and 860:
Neuropathic pain - Neuropathic pain
- Page 861 and 862:
• Management Stop antipsychotic
- Page 863 and 864:
Lamotrogine (lamictal) • Uses : A
- Page 865 and 866:
1
- Page 867 and 868:
- Layers of the eyeball : Sclera :
- Page 869 and 870:
N.B New classification of non-proli
- Page 871 and 872:
Dry (geographic atrophy) macular de
- Page 873 and 874:
B. Congenital causes 1. Friedreich'
- Page 875 and 876:
Acute angle closure glaucoma - In a
- Page 877 and 878:
سؤال هام فى االمتحا
- Page 879 and 880:
Relative afferent pupillary defect
- Page 881 and 882:
Homocystinuria - Homocystinuria is
- Page 883 and 884:
Causes of bilateral ptosis 5. Myoto
- Page 885 and 886:
1
- Page 887 and 888:
- When a drug is administrated to t
- Page 889 and 890:
2) Binding to plasma & tissue prote
- Page 891 and 892:
- Metabolism of the drugs ccurs in
- Page 893 and 894:
Metabolism of paracetamol in overdo
- Page 895 and 896:
Management of paracetamol toxicity
- Page 897 and 898:
NB : the most helpful test in deter
- Page 899 and 900:
King's College Hospital criteria fo
- Page 901 and 902:
• Time course of drug metabolism
- Page 903 and 904:
Measurement of plasma drug level :
- Page 905 and 906:
Digoxin and digoxin toxicity - Digo
- Page 907 and 908:
Ectasy (= MDMA = Methylene-dioxy-me
- Page 909 and 910:
Mood disorders Depression • Def :
- Page 911 and 912:
Psychotic depression : - Major depr
- Page 913 and 914:
More sedative Amitriptyline Clomi
- Page 915 and 916:
• Discontinuation symptoms 1) Inc
- Page 917 and 918:
• Examples of typical antipsychot
- Page 919 and 920:
• Treatment of bipolar disorder :
- Page 921 and 922:
Lithium - Lithium is a mood stabili
- Page 923 and 924:
Post partum mental health problems
- Page 925 and 926:
Functional deterioration : 1) Impai
- Page 927 and 928:
B. Compulsions : - Stereotyped acti
- Page 929 and 930:
Generalized anxiety disorder (GAD)
- Page 931 and 932:
Somatoform disorders (unexplained s
- Page 933 and 934:
Eating disorders 1. Anorexia nervos
- Page 935 and 936:
Sleep disorders 1. Sleep paralysis
- Page 937 and 938:
• Mechanism : • Features : Subs
- Page 939:
• Diagnosis : Chronic fatigue syn
- Page 942 and 943:
- Causes of defective lung perfusio
- Page 944 and 945:
1) Central regulatory centres : A)
- Page 946 and 947:
Lung capacities :
- Page 948 and 949:
Functional Residual Capacity (FRC)
- Page 950 and 951:
FEV1 Meaning (units) Description Fo
- Page 952 and 953:
هام جداPFT Algorithm of inter
- Page 954 and 955:
Interpretation of flow volume loope
- Page 956 and 957:
Bronchial asthma - BA is a reversib
- Page 958 and 959:
Diagnosis of BA in adults(British T
- Page 960:
Step 4 Step 5 Consider trials of:
- Page 963 and 964:
Causes : 1. Smoking (tobacco smooki
- Page 965 and 966:
The severity of COPD is categorised
- Page 967 and 968:
2. Bronchodilator therapy A short-
- Page 969 and 970:
Bronchiolitis oblitrans(BO) - Progr
- Page 971 and 972:
Extrinsic allergic alveolitis (=hyp
- Page 973 and 974:
Subtypes a) Cylindrical (bronchi ha
- Page 975 and 976:
Cystic fibrosis(CF) - Autosomal rec
- Page 977 and 978:
Pulmonary embolism (PE) - PE is pre
- Page 979 and 980:
CTPA or V/Q scan? The British Thor
- Page 981 and 982:
Management of PE (The NICE guidelin
- Page 983 and 984:
1- General constitutional symptoms
- Page 985 and 986:
Mycoplasma pneumonia - Is a cause o
- Page 987 and 988:
Investigation األهم diagnosis.
- Page 989 and 990:
Aspergilloma : - A fungus ball that
- Page 991 and 992:
Asbestos-related lung diseases Pleu
- Page 993 and 994:
• Clinical features : Dyspnoea
- Page 995 and 996:
• Investigations (NICE 2015) : Sy
- Page 997 and 998:
Stage IIIb Stage IV T1 N0 - No L.N
- Page 999 and 1000:
Non-small cell carcinoma : Squamous
- Page 1001 and 1002:
Lung carcinoid - Neuro-endocrine tu
- Page 1003 and 1004:
Pulmonary eosinophelia - Group of d
- Page 1005 and 1006:
• Investigations : - There is no
- Page 1007 and 1008:
Pleural diseases Pleural effusion -
- Page 1009 and 1010:
3) Pleural(Abram`s) biopsy : - Indi
- Page 1011 and 1012:
• Investigations : 1) Chest X-ray
- Page 1013 and 1014:
- Tension pneumothorax ► Tension
- Page 1015 and 1016:
Respiratory questions reveiw for MR
- Page 1017 and 1018:
Q6 : A 63-year-old woman presents a
- Page 1020 and 1021:
Evaluation & diagnosis of a case of
- Page 1022 and 1023:
- It`s a common degenerative joint
- Page 1024 and 1025:
Cervical spondylosis - It`s an age-
- Page 1026 and 1027:
Rheumatoid arthritis (RA) • Def :
- Page 1028 and 1029:
c) Boutonniere deformity (i.e exten
- Page 1030 and 1031:
هام جدا : arthritis • Diagn
- Page 1032 and 1033:
Methotrexate: - Methotrexate is an
- Page 1034 and 1035:
Ankylosing spondilitis - One of HLA
- Page 1036 and 1037:
• Management of AS: - Early diagn
- Page 1038 and 1039:
The table below shows the organisms
- Page 1040 and 1041:
Behcet's syndrome Behcet's syndrome
- Page 1042 and 1043:
Crystal-induced arthritis GOUT - Go
- Page 1044 and 1045:
IV. Gouty nephropathy : Acute gout
- Page 1046 and 1047:
C. Lifestyle modifications: 1. Redu
- Page 1048 and 1049:
Dermatomyositis • Def : - Inflamm
- Page 1050 and 1051:
Inclusion body myositis (IBM) : - T
- Page 1052 and 1053:
34
- Page 1054 and 1055:
firm surface or flexed for extended
- Page 1056 and 1057:
Ottawa rules: Def : - Are a set of
- Page 1058 and 1059:
Autoimmune rheumatic diseases Syste
- Page 1060 and 1061:
J. Neurological : 1. Lupus cerebrit
- Page 1062 and 1063:
سؤال امتحان Discoid lupu
- Page 1064 and 1065:
• Investigations : 1. Thrombocyto
- Page 1066 and 1067:
• Antibodies: ANA positive in 90
- Page 1068 and 1069:
Sjogren's syndrome - It is an autoi
- Page 1070 and 1071:
Large vessel vasculitis Giant cell
- Page 1072 and 1073:
• Investigations : ( there is no
- Page 1074 and 1075:
Small vessel vasculitis ANCA +VE (
- Page 1076 and 1077:
ANCA -VE vasculitis : Henoch-Schonl
- Page 1078 and 1079:
Disorder Wegener`s granulomatosis G
- Page 1080 and 1081:
Referral to specialist CFS : - With
- Page 1082:
Leflunomide : • Mechanism of acti