chapter viii wool & wollen textiles industry - Ministry of Textiles
chapter viii wool & wollen textiles industry - Ministry of Textiles
chapter viii wool & wollen textiles industry - Ministry of Textiles
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
annual report 2011-12<br />
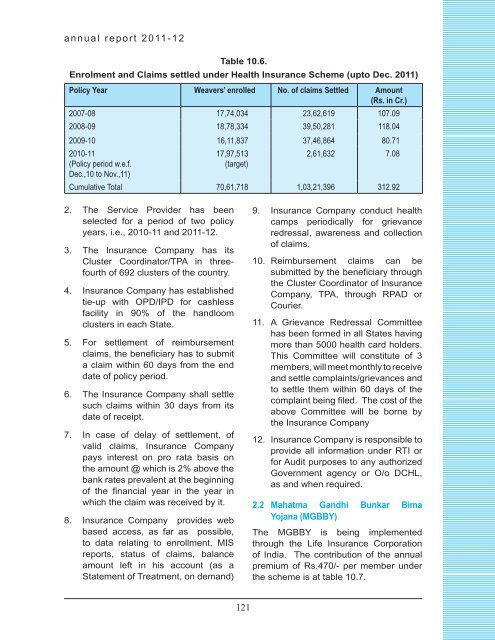
Table 10.6.<br />
Enrolment and Claims settled under Health Insurance Scheme (upto Dec. 2011)<br />
Policy Year Weavers’ enrolled No. <strong>of</strong> claims Settled Amount<br />
(Rs. in Cr.)<br />
2007-08 17,74,034 23,62,619 107.09<br />
2008-09 18,78,334 39,50,281 118.04<br />
2009-10 16,11,837 37,46,864 80.71<br />
2010-11<br />
17,97,513<br />
2,61,632 7.08<br />
(Policy period w.e.f.<br />
Dec.,10 to Nov.,11)<br />
(target)<br />
Cumulative Total 70,61,718 1,03,21,396 312.92<br />
2. The Service Provider has been<br />
selected for a period <strong>of</strong> two policy<br />
years, i.e., 2010-11 and 2011-12.<br />
3. The Insurance Company has its<br />
Cluster Coordinator/TPA in threefourth<br />
<strong>of</strong> 692 clusters <strong>of</strong> the country.<br />
4. Insurance Company has established<br />
tie-up with OPD/IPD for cashless<br />
facility in 90% <strong>of</strong> the handloom<br />
clusters in each State.<br />
5. For settlement <strong>of</strong> reimbursement<br />
claims, the beneficiary has to submit<br />
a claim within 60 days from the end<br />
date <strong>of</strong> policy period.<br />
6. The Insurance Company shall settle<br />
such claims within 30 days from its<br />
date <strong>of</strong> receipt.<br />
7. In case <strong>of</strong> delay <strong>of</strong> settlement, <strong>of</strong><br />
valid claims, Insurance Company<br />
pays interest on pro rata basis on<br />
the amount @ which is 2% above the<br />
bank rates prevalent at the beginning<br />
<strong>of</strong> the financial year in the year in<br />
which the claim was received by it.<br />
8. Insurance Company provides web<br />
based access, as far as possible,<br />
to data relating to enrollment, MIS<br />
reports, status <strong>of</strong> claims, balance<br />
amount left in his account (as a<br />
Statement <strong>of</strong> Treatment, on demand)<br />
9. Insurance Company conduct health<br />
camps periodically for grievance<br />
redressal, awareness and collection<br />
<strong>of</strong> claims.<br />
10. Reimbursement claims can be<br />
submitted by the beneficiary through<br />
the Cluster Coordinator <strong>of</strong> Insurance<br />
Company, TPA, through RPAD or<br />
Courier.<br />
11. A Grievance Redressal Committee<br />
has been formed in all States having<br />
more than 5000 health card holders.<br />
This Committee will constitute <strong>of</strong> 3<br />
members, will meet monthly to receive<br />
and settle complaints/grievances and<br />
to settle them within 60 days <strong>of</strong> the<br />
complaint being filed. The cost <strong>of</strong> the<br />
above Committee will be borne by<br />
the Insurance Company<br />
12. Insurance Company is responsible to<br />
provide all information under RTI or<br />
for Audit purposes to any authorized<br />
Government agency or O/o DCHL,<br />
as and when required.<br />
2.2 Mahatma Gandhi Bunkar Bima<br />
Yojana (MGBBY)<br />
The MGBBY is being implemented<br />
through the Life Insurance Corporation<br />
<strong>of</strong> India. The contribution <strong>of</strong> the annual<br />
premium <strong>of</strong> Rs.470/- per member under<br />
the scheme is at table 10.7.<br />
121