LVR-Klinikum Düsseldorf Hospital of the Heinrich-Heine University ...
LVR-Klinikum Düsseldorf Hospital of the Heinrich-Heine University ...
LVR-Klinikum Düsseldorf Hospital of the Heinrich-Heine University ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
investigations <strong>of</strong> different questions on <strong>the</strong> optimisation<br />
<strong>of</strong> <strong>the</strong> long-term treatment <strong>of</strong> patients with<br />
schizophrenia (Figure 14):<br />
s Benefits <strong>of</strong> (“atypical”‘) second generation antipsychotic<br />
drugs compared with those <strong>of</strong> <strong>the</strong> first generation<br />
(“typicals”);<br />
s Necessary period <strong>of</strong> continuous maintenance<br />
medication for fur<strong>the</strong>r stabilisation and relapse<br />
prophylaxis;<br />
s Opportunities afforded by an improved use <strong>of</strong><br />
prodromal symptoms for early diagnosis and<br />
intervention;<br />
s Improvement <strong>of</strong> <strong>the</strong> risk estimation for relapses and<br />
residual course developments, as well as<br />
s The effectiveness <strong>of</strong> psychological intervention<br />
strategies with regard to relapse prophylaxis and o<strong>the</strong>r<br />
outcome criteria through <strong>the</strong> modification <strong>of</strong> individual<br />
vulnerability, stress response and coping skills.<br />
Pharmaco<strong>the</strong>rapeutic strategies for relapse prevention in<br />
first-episode patients with schizophrenia<br />
Director: W. Gaebel, H.J. Möller (Psychiatric Department <strong>of</strong><br />
Ludwig-Maximilian <strong>University</strong>, Munich)<br />
Project period: 1999–2005<br />
Financing: FMER funding 01 GI 9932/01 GI 0232<br />
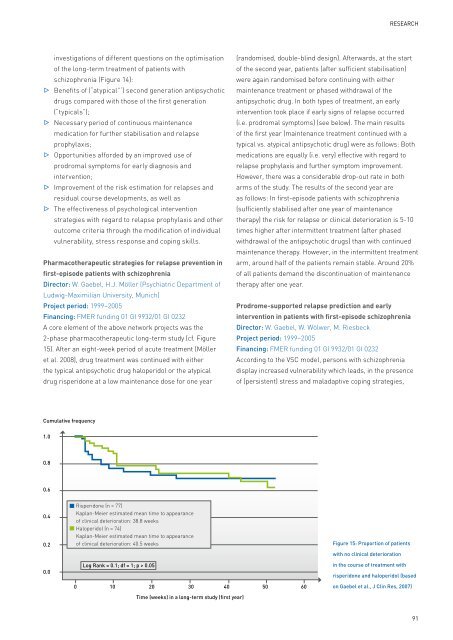
A core element <strong>of</strong> <strong>the</strong> above network projects was <strong>the</strong><br />
2-phase pharmaco<strong>the</strong>rapeutic long-term study (cf. Figure<br />
15). After an eight-week period <strong>of</strong> acute treatment (Möller<br />
et al. 2008), drug treatment was continued with ei<strong>the</strong>r<br />
<strong>the</strong> typical antipsychotic drug haloperidol or <strong>the</strong> atypical<br />
drug risperidone at a low maintenance dose for one year<br />
Cumulative frequency<br />
1.0<br />
0.8<br />
0.6<br />
0.4<br />
0.2<br />
0.0<br />
Risperidone (n = 77)<br />
Kaplan-Meier estimated mean time to appearance<br />
<strong>of</strong> clinical deterioration: 38.8 weeks<br />
Haloperidol (n = 74)<br />
Kaplan-Meier estimated mean time to appearance<br />
<strong>of</strong> clinical deterioration: 40.5 weeks<br />
Log Rank = 0.1; df = 1; p > 0.05<br />
0 10 20 30 40 50 60<br />
Time (weeks) in a long-term study (first year)<br />
ReseaRch<br />
(randomised, double-blind design). Afterwards, at <strong>the</strong> start<br />
<strong>of</strong> <strong>the</strong> second year, patients (after sufficient stabilisation)<br />
were again randomised before continuing with ei<strong>the</strong>r<br />
maintenance treatment or phased withdrawal <strong>of</strong> <strong>the</strong><br />
antipsychotic drug. In both types <strong>of</strong> treatment, an early<br />
intervention took place if early signs <strong>of</strong> relapse occurred<br />
(i.e. prodromal symptoms) (see below). The main results<br />
<strong>of</strong> <strong>the</strong> first year (maintenance treatment continued with a<br />
typical vs. atypical antipsychotic drug) were as follows: Both<br />
medications are equally (i.e. very) effective with regard to<br />
relapse prophylaxis and fur<strong>the</strong>r symptom improvement.<br />
However, <strong>the</strong>re was a considerable drop-out rate in both<br />
arms <strong>of</strong> <strong>the</strong> study. The results <strong>of</strong> <strong>the</strong> second year are<br />
as follows: In first-episode patients with schizophrenia<br />
(sufficiently stabilised after one year <strong>of</strong> maintenance<br />
<strong>the</strong>rapy) <strong>the</strong> risk for relapse or clinical deterioration is 5-10<br />
times higher after intermittent treatment (after phased<br />
withdrawal <strong>of</strong> <strong>the</strong> antipsychotic drugs) than with continued<br />
maintenance <strong>the</strong>rapy. However, in <strong>the</strong> intermittent treatment<br />
arm, around half <strong>of</strong> <strong>the</strong> patients remain stable. Around 20%<br />
<strong>of</strong> all patients demand <strong>the</strong> discontinuation <strong>of</strong> maintenance<br />
<strong>the</strong>rapy after one year.<br />
Prodrome-supported relapse prediction and early<br />
intervention in patients with first-episode schizophrenia<br />
Director: W. Gaebel, W. Wölwer, M. Riesbeck<br />
Project period: 1999–2005<br />
Financing: FMER funding 01 GI 9932/01 GI 0232<br />
According to <strong>the</strong> VSC model, persons with schizophrenia<br />
display increased vulnerability which leads, in <strong>the</strong> presence<br />
<strong>of</strong> (persistent) stress and maladaptive coping strategies,<br />
Figure 15: Proportion <strong>of</strong> patients<br />
with no clinical deterioration<br />
in <strong>the</strong> course <strong>of</strong> treatment with<br />
risperidone and haloperidol (based<br />
on Gaebel et al., J Clin Res, 2007)<br />
91