Quelles solutions pour la garde en médecine générale? - KCE
Quelles solutions pour la garde en médecine générale? - KCE
Quelles solutions pour la garde en médecine générale? - KCE
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
104<br />
8.4.2. After-hhours<br />
care in Thhe<br />
United Kingdo om<br />
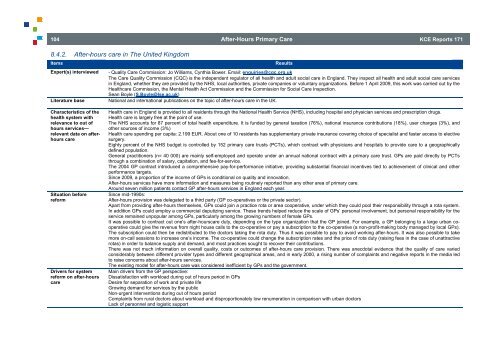
Items<br />
Expert(s) interviewwed<br />
- Quality Caree<br />
Commission: Jo Williams,<br />
Cynthia Bower. . Email: <strong>en</strong>quiries@cqqc.org.uk <br />
The Care Quuality<br />
Commission (CQ QC) is the indep<strong>en</strong>d<strong>en</strong>nt<br />
regu<strong>la</strong>tor of all healtth<br />
and adult social care<br />
in Eng<strong>la</strong>nd. They innspect<br />
all health and aadult<br />
social care serviices<br />
in Eng<strong>la</strong>nd, wwhether<br />
they are provided<br />
by the NHS, locall<br />
authorities, private coompanies<br />
or voluntaryy<br />
organizations. Beforee<br />
1 April 2009, this woork<br />
was carried out by the<br />
Healthcare CCommission,<br />
the M<strong>en</strong>ta al Health Act Commisssion<br />
and the Commisssion<br />
for Social Care Innspection.<br />
Sean Boyle ( S.Boyle@lse.ac.uk)<br />
Literature base<br />
National and international publications<br />
on the topic of aftter-hours<br />
care in the UUK.<br />
Characteristics off<br />
the<br />
health system with<br />
relevance to out oof<br />
hours services—<br />
relevant data on aafter-<br />
hours care<br />
Situation before<br />
reform<br />
Drivers for systemm<br />
reform on after-hoours<br />
care<br />
Affter-Hours<br />
Primaary<br />
Care<br />
Results<br />
<strong>KCE</strong> Reportss<br />
171<br />
Health care inn<br />
Eng<strong>la</strong>nd is provided to all resid<strong>en</strong>ts througgh<br />
the National Healthh<br />
Service (NHS), includding<br />
hospital and physsician<br />
services and prrescription<br />
drugs.<br />
Health care iss<br />
<strong>la</strong>rgely free at the po oint of use.<br />
The NHS acccounts<br />
for 87 perc<strong>en</strong>t of total health exp<strong>en</strong>diture.<br />
It is funded byy<br />
g<strong>en</strong>eral taxation (76% %), national insurancee<br />
contributions (18%) , user charges (3%), and<br />
other sourcess<br />
of income (3%)<br />
Health care ssp<strong>en</strong>ding<br />
per capita: 2.199<br />
EUR. About one of 10 resid<strong>en</strong>ts has supplem<strong>en</strong>tary<br />
private insurance covering chhoice<br />
of specialist andd<br />
faster access to elecctive<br />
surgery.<br />
Eighty perc<strong>en</strong>nt<br />
of the NHS budget t is controlled by 152 primary care trusts ( PCTs), which contracct<br />
with physicians andd<br />
hospitals to provide care to a geographiccally<br />
defined popu<strong>la</strong>tion.<br />
G<strong>en</strong>eral pracctitioners<br />
(n= 40 000) are mainly self-emplooyed<br />
and operate undder<br />
an annual nationaal<br />
contract with a primmary<br />
care trust. GPs aare<br />
paid directly by PCCTs<br />
through a commbination<br />
of sa<strong>la</strong>ry, ca apitation, and fee-for-sservice.<br />
The 2004 GPP<br />
contract introduced a compreh<strong>en</strong>sive payy-for-performance<br />
inittiative,<br />
providing subsstantial<br />
financial inc<strong>en</strong>tives<br />
tied to achievemm<strong>en</strong>t<br />
of clinical and otther<br />
performance targets.<br />
Since 2009, a proportion of the income<br />
of GPs is conditioonal<br />
on quality and innnovation.<br />
After-hours services<br />
have more inf formation and measurees<br />
being routinely reported<br />
than any other aarea<br />
of primary care.<br />
Around sev<strong>en</strong>n<br />
million pati<strong>en</strong>ts contact<br />
GP after-hours services<br />
in Eng<strong>la</strong>nd each<br />
year.<br />
Since mid-19990s:<br />
After-hours pprovision<br />
was delegate ed to a third party (GP co-operatives or the pprivate<br />
sector).<br />
Apart from prroviding<br />
after-hours th hemselves, GPs could join a practice rota orr<br />
area cooperative, unnder<br />
which they could pool their responsibiliity<br />
through a rota system.<br />
In addition GPs<br />
could employ a co ommercial deputizing sservice.<br />
These tr<strong>en</strong>ds helped reduce the sccale<br />
of GPs’ personal involvem<strong>en</strong>t, but personal<br />
responsibility for the<br />
service remained<br />
unpopu<strong>la</strong>r among g GPs, particu<strong>la</strong>rly ammong<br />
the growing numbers<br />
of female GPs.<br />
It was possibble<br />
to contract out one e’s after-hourscare duuty,<br />
dep<strong>en</strong>ding on the type organization thaat<br />
the GP joined. For eexample,<br />
a GP belonging<br />
to a <strong>la</strong>rge urban cooperative<br />
couuld<br />
give the rev<strong>en</strong>ue fr rom night house calls to the co-operative orr<br />
pay a subscription to the co-operative (a non-profit-making<br />
bodyy<br />
managed by local GPPs).<br />
The subscripption<br />
could th<strong>en</strong> be red distributed to the docttors<br />
taking the rota duuty.<br />
Thus it was possible<br />
to pay to avoid woorking<br />
after-hours. It wwas<br />
also possible to ttake<br />
more on-call sessions to increase one’s o income. The co-operative<br />
could change<br />
the subscription raates<br />
and the price of roota<br />
duty (raising fees in<br />
the case of unattracctive<br />
rotas) in ordeer<br />
to ba<strong>la</strong>nce supply an nd demand, and mostt<br />
practices sought to reecover<br />
their contributioons.<br />
There was not<br />
much information on overall quality, costs<br />
or outcomes of aafter-hours<br />
care provission.<br />
There was aneccdotal<br />
evid<strong>en</strong>ce that the<br />
quality of care varied<br />
considerably betwe<strong>en</strong> differ<strong>en</strong>t pro ovider types and differ<strong>en</strong>t<br />
geographical areaas,<br />
and in early 2000, a rising number of coomp<strong>la</strong>ints<br />
and negativee<br />
reports in the media led<br />
to raise conceerns<br />
about after-hours s services.<br />
The existing model for after-hours care was considered iineffici<strong>en</strong>t<br />
by GPs andd<br />
the governm<strong>en</strong>t.<br />
Main drivers from the GP perspective:<br />
Dissatisfactioon<br />
with workload during<br />
out of hours period in GPs<br />
Desire for separation<br />
of work and private p life<br />
Growing demmand<br />
for services by th he public<br />
Non-urg<strong>en</strong>t innterv<strong>en</strong>tions<br />
during ou ut of hours period<br />
Comp<strong>la</strong>ints frrom<br />
rural doctors abou ut workload and disprooportionately<br />
low r<strong>en</strong>uumeration<br />
in comparisoon<br />
with urban doctors<br />
Lack of persoonnel<br />
and logistic supp port