- Page 2 and 3:
Reproduction in Domestic AnimalsOff
- Page 5 and 6:
Reproductionin Domestic AnimalsTabl
- Page 7 and 8:
Minitüb:ProductsforArtificial Inse
- Page 9 and 10:
Reprod Dom Anim 43 (Suppl. 2), 1-7
- Page 11 and 12:
Embryo Biotechnologies in Farm Anim
- Page 13 and 14:
Embryo Biotechnologies in Farm Anim
- Page 15 and 16:
Embryo Biotechnologies in Farm Anim
- Page 17 and 18:
Ethical Models for Studying Reprodu
- Page 19 and 20:
Ethical Models for Studying Reprodu
- Page 21 and 22:
Ethical Models for Studying Reprodu
- Page 23 and 24:
Reprod Dom Anim 43 (Suppl. 2), 15-2
- Page 25 and 26:
Dietary Pollutants as Risk Factors
- Page 27 and 28:
Dietary Pollutants as Risk Factors
- Page 29 and 30:
Dietary Pollutants as Risk Factors
- Page 31 and 32:
Reprod Dom Anim 43 (Supp. 2), 23-30
- Page 33 and 34:
Factors Influencing Reproduction in
- Page 35 and 36:
Factors Influencing Reproduction in
- Page 37 and 38:
Factors Influencing Reproduction in
- Page 39 and 40:
Reprod Dom Anim 43 (Suppl. 2), 31-3
- Page 41 and 42:
GH and IGF-I in Cattle and Pigs 33h
- Page 43 and 44:
GH and IGF-I in Cattle and Pigs 35h
- Page 45 and 46:
GH and IGF-I in Cattle and Pigs 37B
- Page 47:
GH and IGF-I in Cattle and Pigs 39R
- Page 51 and 52:
Seasonality of Reproduction in Mamm
- Page 53 and 54:
Seasonality of Reproduction in Mamm
- Page 55 and 56:
Seasonality of Reproduction in Mamm
- Page 57 and 58:
Dominant Follicle Selection in Cows
- Page 59 and 60:
Dominant Follicle Selection in Cows
- Page 61 and 62:
Dominant Follicle Selection in Cows
- Page 63 and 64:
Dominant Follicle Selection in Cows
- Page 65 and 66: Reprod Dom Anim 43 (Suppl. 2), 57-6
- Page 67 and 68: Regulation of Luteal Function 59and
- Page 69 and 70: Regulation of Luteal Function 61bov
- Page 71 and 72: Regulation of Luteal Function 63(+/
- Page 73 and 74: Regulation of Luteal Function 65sys
- Page 75 and 76: Captive Breeding of Cheetahs in Sou
- Page 77 and 78: Captive Breeding of Cheetahs in Sou
- Page 79 and 80: Captive Breeding of Cheetahs in Sou
- Page 81 and 82: Captive Breeding of Cheetahs in Sou
- Page 83 and 84: Non-invasive Monitoring of Hormones
- Page 85 and 86: Non-invasive Monitoring of Hormones
- Page 87 and 88: Non-invasive Monitoring of Hormones
- Page 89 and 90: Non-invasive Monitoring of Hormones
- Page 91 and 92: Reprod Dom Anim 43 (Suppl. 2), 83-8
- Page 93 and 94: Biotechnology Methods for Preservin
- Page 95 and 96: Biotechnology Methods for Preservin
- Page 97 and 98: Reprod Dom Anim 43 (Suppl. 2), 89-9
- Page 99 and 100: Genetic Improvement of Dairy Cow Re
- Page 101 and 102: Genetic Improvement of Dairy Cow Re
- Page 103 and 104: Genetic Improvement of Dairy Cow Re
- Page 105 and 106: Nutrient Prioritization and Fertili
- Page 107 and 108: Nutrient Prioritization and Fertili
- Page 109 and 110: Nutrient Prioritization and Fertili
- Page 111 and 112: Nutrient Prioritization and Fertili
- Page 113 and 114: CL-Endometrium-Embryo Interactions
- Page 115: CL-Endometrium-Embryo Interactions
- Page 119 and 120: CL-Endometrium-Embryo Interactions
- Page 121 and 122: Reprod Dom Anim 43 (Suppl. 2), 113-
- Page 123 and 124: Reproductive Status Assessed by Mil
- Page 125 and 126: Reproductive Status Assessed by Mil
- Page 127 and 128: Reproductive Status Assessed by Mil
- Page 129 and 130: Reproductive Status Assessed by Mil
- Page 131 and 132: Genetic Aspects of Reproduction in
- Page 133 and 134: Genetic Aspects of Reproduction in
- Page 135 and 136: Genetic Aspects of Reproduction in
- Page 137 and 138: Reprod Dom Anim 43 (Suppl. 2), 129-
- Page 139 and 140: Nutritional Interactions and Reprod
- Page 141 and 142: Nutritional Interactions and Reprod
- Page 143 and 144: Nutritional Interactions and Reprod
- Page 145 and 146: Reprod Dom Anim 43 (Suppl. 2), 137-
- Page 147 and 148: Developmental Capabilities of Prepu
- Page 149 and 150: Developmental Capabilities of Prepu
- Page 151 and 152: Developmental Capabilities of Prepu
- Page 153 and 154: Reproductive Physiology, Pathology
- Page 155 and 156: Reproductive Physiology, Pathology
- Page 157 and 158: Reproductive Physiology, Pathology
- Page 159 and 160: Reproduction of Domestic Ferret 151
- Page 161 and 162: Reproduction of Domestic Ferret 153
- Page 163 and 164: Reproduction of Domestic Ferret 155
- Page 165 and 166: Reprod Dom Anim 43 (Suppl. 2), 157-
- Page 167 and 168:
Canine Anoestrus, Oestrous Inductio
- Page 169 and 170:
Canine Anoestrus, Oestrous Inductio
- Page 171 and 172:
Canine Anoestrus, Oestrous Inductio
- Page 173 and 174:
Reprod Dom Anim 43 (Suppl. 2), 165-
- Page 175 and 176:
The Ethics and Role of AI in Dogs 1
- Page 177 and 178:
The Ethics and Role of AI in Dogs 1
- Page 179 and 180:
The Ethics and Role of AI in Dogs 1
- Page 181 and 182:
Control of Fertility in Females by
- Page 183 and 184:
Control of Fertility in Females by
- Page 185 and 186:
Control of Fertility in Females by
- Page 187 and 188:
Reprod Dom Anim 43 (Suppl. 2), 179-
- Page 189 and 190:
Controlling Animal Populations Usin
- Page 191 and 192:
Controlling Animal Populations Usin
- Page 193 and 194:
Controlling Animal Populations Usin
- Page 195 and 196:
Recombinant Gonadotropins in Assist
- Page 197 and 198:
Recombinant Gonadotropins in Assist
- Page 199 and 200:
Recombinant Gonadotropins in Assist
- Page 201 and 202:
Reprod Dom Anim 43 (Suppl. 2), 193-
- Page 203 and 204:
Farm Animals Embryonic Stem Cells 1
- Page 205 and 206:
Farm Animals Embryonic Stem Cells 1
- Page 207 and 208:
Farm Animals Embryonic Stem Cells 1
- Page 209 and 210:
Reproduction in Domestic Buffalo 20
- Page 211 and 212:
Reproduction in Domestic Buffalo 20
- Page 213 and 214:
Reproduction in Domestic Buffalo 20
- Page 215 and 216:
Reprod Dom Anim 43 (Suppl. 2), 207-
- Page 217 and 218:
Postpartum Ovarian Activity in Sout
- Page 219 and 220:
Postpartum Ovarian Activity in Sout
- Page 221 and 222:
Reprod Dom Anim 43 (Suppl. 2), 213-
- Page 223 and 224:
Mother-Offspring Interactions 215an
- Page 225 and 226:
Reprod Dom Anim 43 (Suppl. 2), 217-
- Page 227 and 228:
Reproduction Augmentation in Yak an
- Page 229 and 230:
Reproduction Augmentation in Yak an
- Page 231 and 232:
Reproduction Augmentation in Yak an
- Page 233 and 234:
Follicles and Mares 2251982). Simil
- Page 235 and 236:
Follicles and Mares 227Studies invo
- Page 237 and 238:
Follicles and Mares 229dominant fol
- Page 239 and 240:
Follicles and Mares 231trus, spring
- Page 241 and 242:
Proteins in Early Equine Conceptuse
- Page 243 and 244:
Proteins in Early Equine Conceptuse
- Page 245 and 246:
Proteins in Early Equine Conceptuse
- Page 247 and 248:
Follicular and Oocyte Competence un
- Page 249 and 250:
Follicular and Oocyte Competence un
- Page 251 and 252:
Follicular and Oocyte Competence un
- Page 253 and 254:
Reprod Dom Anim 43 (Suppl. 2), 245-
- Page 255 and 256:
Fertilization in the Porcine Fallop
- Page 257 and 258:
Fertilization in the Porcine Fallop
- Page 259 and 260:
Fertilization in the Porcine Fallop
- Page 261 and 262:
Mastitis in Post-Partum Dairy Cows
- Page 263 and 264:
Mastitis in Post-Partum Dairy Cows
- Page 265 and 266:
Mastitis in Post-Partum Dairy Cows
- Page 267 and 268:
Mastitis in Post-Partum Dairy Cows
- Page 269 and 270:
Embryo ⁄ Foetal Losses in Ruminan
- Page 271 and 272:
Embryo ⁄ Foetal Losses in Ruminan
- Page 273 and 274:
Embryo ⁄ Foetal Losses in Ruminan
- Page 275 and 276:
Embryo ⁄ Foetal Losses in Ruminan
- Page 277 and 278:
Death Ligand and Receptor Pig Ovari
- Page 279 and 280:
Death Ligand and Receptor Pig Ovari
- Page 281 and 282:
Reprod Dom Anim 43 (Suppl. 2), 273-
- Page 283:
Lactocrine Programming of Uterine D
- Page 286 and 287:
278 FF Bartol, AA Wiley and CA Bagn
- Page 288 and 289:
Reprod Dom Anim 43 (Suppl. 2), 280-
- Page 290 and 291:
282 KC Caires, JA Schmidt, AP Olive
- Page 292 and 293:
284 KC Caires, JA Schmidt, AP Olive
- Page 294 and 295:
286 KC Caires, JA Schmidt, AP Olive
- Page 296 and 297:
Reprod Dom Anim 43 (Suppl. 2), 288-
- Page 298 and 299:
290 I Dobrinskisuccessful also betw
- Page 300 and 301:
292 I DobrinskiCreemers LB, Meng X,
- Page 302 and 303:
294 I DobrinskiOkutsu T, Suzuki K,
- Page 304 and 305:
296 N Rawlings, ACO Evans, RK Chand
- Page 306 and 307:
298 N Rawlings, ACO Evans, RK Chand
- Page 308 and 309:
300 N Rawlings, ACO Evans, RK Chand
- Page 310 and 311:
Reprod Dom Anim 43 (Suppl. 2), 302-
- Page 312 and 313:
304 A Dinnyes, XC Tian and X Yanggr
- Page 314 and 315:
306 A Dinnyes, XC Tian and X YangIn
- Page 316 and 317:
308 A Dinnyes, XC Tian and X YangHo
- Page 318 and 319:
Reprod Dom Anim 43 (Suppl. 2), 310-
- Page 320 and 321:
312 RC Bott, DT Clopton and AS Cupp
- Page 322 and 323:
314 RC Bott, DT Clopton and AS Cupp
- Page 324 and 325:
316 RC Bott, DT Clopton and AS Cupp
- Page 326 and 327:
318 BK Whitlock, JA Daniel, RR Wilb
- Page 328 and 329:
320 BK Whitlock, JA Daniel, RR Wilb
- Page 330 and 331:
322 BK Whitlock, JA Daniel, RR Wilb
- Page 332 and 333:
Reprod Dom Anim 43 (Suppl. 2), 324-
- Page 334 and 335:
326 CR Barb, GJ Hausman and CA Lent
- Page 336 and 337:
328 CR Barb, GJ Hausman and CA Lent
- Page 338 and 339:
330 CR Barb, GJ Hausman and CA Lent
- Page 340 and 341:
332 C Galli, I Lagutina, R Duchi, S
- Page 342 and 343:
334 C Galli, I Lagutina, R Duchi, S
- Page 344 and 345:
336 C Galli, I Lagutina, R Duchi, S
- Page 346 and 347:
Reprod Dom Anim 43 (Suppl. 2), 338-
- Page 348 and 349:
340 D Rath and LA JohnsonCommercial
- Page 350 and 351:
342 D Rath and LA JohnsonThe Commer
- Page 352 and 353:
344 D Rath and LA JohnsonX- and Y-b
- Page 354 and 355:
346 D Rath and LA JohnsonWalker SK,
- Page 356 and 357:
348 JM Vazquez, J Roca, MA Gil, C C
- Page 358 and 359:
350 JM Vazquez, J Roca, MA Gil, C C
- Page 360 and 361:
352 JM Vazquez, J Roca, MA Gil, C C
- Page 362 and 363:
354 JM Vazquez, J Roca, MA Gil, C C
- Page 364 and 365:
356 CBA Whitelaw, SG Lillico and T
- Page 366 and 367:
358 CBA Whitelaw, SG Lillico and T
- Page 368 and 369:
360 ACO Evans, N Forde, GM O’Gorm
- Page 370 and 371:
362 ACO Evans, N Forde, GM O’Gorm
- Page 372 and 373:
364 ACO Evans, N Forde, GM O’Gorm
- Page 374 and 375:
366 ACO Evans, N Forde, GM O’Gorm
- Page 376 and 377:
Reprod Dom Anim 43 (Suppl. 2), 368-
- Page 378 and 379:
370 JP Kastelic and JC Thundathilsp
- Page 380 and 381:
372 JP Kastelic and JC Thundathilme
- Page 382 and 383:
Reprod Dom Anim 43 (Suppl. 2), 374-
- Page 384 and 385:
376 GC AlthouseTable 1. Potential s
- Page 386 and 387:
378 GC Althousesemen to the domesti
- Page 388 and 389:
380 B Leboeuf, JA Delgadillo, E Man
- Page 390 and 391:
382 B Leboeuf, JA Delgadillo, E Man
- Page 392 and 393:
384 B Leboeuf, JA Delgadillo, E Man
- Page 394 and 395:
Reprod Dom Anim 43 (Suppl. 2), 386-
- Page 396 and 397:
388 N Kostereva and M-C HofmannFig.
- Page 398 and 399:
390 N Kostereva and M-C HofmannMMPs
- Page 400 and 401:
392 N Kostereva and M-C HofmannTado
- Page 402 and 403:
394 P Mermillod, R Dalbie` s-Tran,
- Page 404 and 405:
396 P Mermillod, R Dalbie` s-Tran,
- Page 406 and 407:
398 P Mermillod, R Dalbie` s-Tran,
- Page 408 and 409:
400 P Mermillod, R Dalbie` s-Tran,
- Page 410 and 411:
402 K Kikuchi, N Kashiwazaki, T Nag
- Page 412 and 413:
404 K Kikuchi, N Kashiwazaki, T Nag
- Page 414 and 415:
406 K Kikuchi, N Kashiwazaki, T Nag
- Page 416 and 417:
408 B ObackNumber of publications20
- Page 418 and 419:
410 B ObackReprogramming Ability of
- Page 420 and 421:
412 B Obackstudies have shown that
- Page 422 and 423:
414 B ObackFig. 4. Climbing mount e
- Page 424 and 425:
416 B ObackRenard JP, Maruotti J, J
- Page 426 and 427:
418 P Loi, K Matzukawa, G Ptak, Y N
- Page 428 and 429:
420 P Loi, K Matzukawa, G Ptak, Y N
- Page 430 and 431:
422 P Loi, K Matzukawa, G Ptak, Y N
- Page 434:
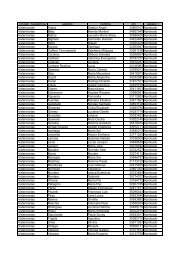
Table of Contents Volume 43 · Supp