Reproduction in Domestic Animals
Reproduction in Domestic Animals
Reproduction in Domestic Animals
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
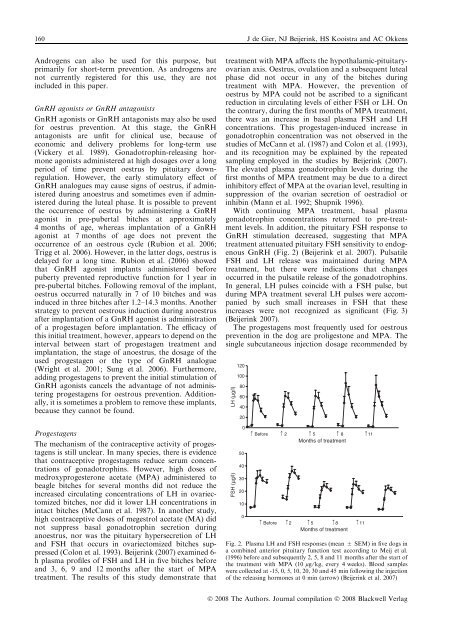
160 J de Gier, NJ Beijer<strong>in</strong>k, HS Kooistra and AC OkkensAndrogens can also be used for this purpose, butprimarily for short-term prevention. As androgens arenot currently registered for this use, they are not<strong>in</strong>cluded <strong>in</strong> this paper.GnRH agonists or GnRH antagonistsGnRH agonists or GnRH antagonists may also be usedfor oestrus prevention. At this stage, the GnRHantagonists are unfit for cl<strong>in</strong>ical use, because ofeconomic and delivery problems for long-term use(Vickery et al. 1989). Gonadotroph<strong>in</strong>-releas<strong>in</strong>g hormoneagonists adm<strong>in</strong>istered at high dosages over a longperiod of time prevent oestrus by pituitary downregulation.However, the early stimulatory effect ofGnRH analogues may cause signs of oestrus, if adm<strong>in</strong>istereddur<strong>in</strong>g anoestrus and sometimes even if adm<strong>in</strong>istereddur<strong>in</strong>g the luteal phase. It is possible to preventthe occurrence of oestrus by adm<strong>in</strong>ister<strong>in</strong>g a GnRHagonist <strong>in</strong> pre-pubertal bitches at approximately4 months of age, whereas implantation of a GnRHagonist at 7 months of age does not prevent theoccurrence of an oestrous cycle (Rubion et al. 2006;Trigg et al. 2006). However, <strong>in</strong> the latter dogs, oestrus isdelayed for a long time. Rubion et al. (2006) showedthat GnRH agonist implants adm<strong>in</strong>istered beforepuberty prevented reproductive function for 1 year <strong>in</strong>pre-pubertal bitches. Follow<strong>in</strong>g removal of the implant,oestrus occurred naturally <strong>in</strong> 7 of 10 bitches and was<strong>in</strong>duced <strong>in</strong> three bitches after 1.2–14.3 months. Anotherstrategy to prevent oestrous <strong>in</strong>duction dur<strong>in</strong>g anoestrusafter implantation of a GnRH agonist is adm<strong>in</strong>istrationof a progestagen before implantation. The efficacy ofthis <strong>in</strong>itial treatment, however, appears to depend on the<strong>in</strong>terval between start of progestagen treatment andimplantation, the stage of anoestrus, the dosage of theused progestagen or the type of GnRH analogue(Wright et al. 2001; Sung et al. 2006). Furthermore,add<strong>in</strong>g progestagens to prevent the <strong>in</strong>itial stimulation ofGnRH agonists cancels the advantage of not adm<strong>in</strong>ister<strong>in</strong>gprogestagens for oestrous prevention. Additionally,it is sometimes a problem to remove these implants,because they cannot be found.ProgestagensThe mechanism of the contraceptive activity of progestagensis still unclear. In many species, there is evidencethat contraceptive progestagens reduce serum concentrationsof gonadotroph<strong>in</strong>s. However, high doses ofmedroxyprogesterone acetate (MPA) adm<strong>in</strong>istered tobeagle bitches for several months did not reduce the<strong>in</strong>creased circulat<strong>in</strong>g concentrations of LH <strong>in</strong> ovariectomizedbitches, nor did it lower LH concentrations <strong>in</strong><strong>in</strong>tact bitches (McCann et al. 1987). In another study,high contraceptive doses of megestrol acetate (MA) didnot suppress basal gonadotroph<strong>in</strong> secretion dur<strong>in</strong>ganoestrus, nor was the pituitary hypersecretion of LHand FSH that occurs <strong>in</strong> ovariectomized bitches suppressed(Colon et al. 1993). Beijer<strong>in</strong>k (2007) exam<strong>in</strong>ed 6-h plasma profiles of FSH and LH <strong>in</strong> five bitches beforeand 3, 6, 9 and 12 months after the start of MPAtreatment. The results of this study demonstrate thattreatment with MPA affects the hypothalamic-pituitaryovarianaxis. Oestrus, ovulation and a subsequent lutealphase did not occur <strong>in</strong> any of the bitches dur<strong>in</strong>gtreatment with MPA. However, the prevention ofoestrus by MPA could not be ascribed to a significantreduction <strong>in</strong> circulat<strong>in</strong>g levels of either FSH or LH. Onthe contrary, dur<strong>in</strong>g the first months of MPA treatment,there was an <strong>in</strong>crease <strong>in</strong> basal plasma FSH and LHconcentrations. This progestagen-<strong>in</strong>duced <strong>in</strong>crease <strong>in</strong>gonadotroph<strong>in</strong> concentration was not observed <strong>in</strong> thestudies of McCann et al. (1987) and Colon et al. (1993),and its recognition may be expla<strong>in</strong>ed by the repeatedsampl<strong>in</strong>g employed <strong>in</strong> the studies by Beijer<strong>in</strong>k (2007).The elevated plasma gonadotroph<strong>in</strong> levels dur<strong>in</strong>g thefirst months of MPA treatment may be due to a direct<strong>in</strong>hibitory effect of MPA at the ovarian level, result<strong>in</strong>g <strong>in</strong>suppression of the ovarian secretion of oestradiol or<strong>in</strong>hib<strong>in</strong> (Mann et al. 1992; Shupnik 1996).With cont<strong>in</strong>u<strong>in</strong>g MPA treatment, basal plasmagonadotroph<strong>in</strong> concentrations returned to pre-treatmentlevels. In addition, the pituitary FSH response toGnRH stimulation decreased, suggest<strong>in</strong>g that MPAtreatment attenuated pituitary FSH sensitivity to endogenousGnRH (Fig. 2) (Beijer<strong>in</strong>k et al. 2007). PulsatileFSH and LH release was ma<strong>in</strong>ta<strong>in</strong>ed dur<strong>in</strong>g MPAtreatment, but there were <strong>in</strong>dications that changesoccurred <strong>in</strong> the pulsatile release of the gonadotroph<strong>in</strong>s.In general, LH pulses co<strong>in</strong>cide with a FSH pulse, butdur<strong>in</strong>g MPA treatment several LH pulses were accompaniedby such small <strong>in</strong>creases <strong>in</strong> FSH that these<strong>in</strong>creases were not recognized as significant (Fig. 3)(Beijer<strong>in</strong>k 2007).The progestagens most frequently used for oestrousprevention <strong>in</strong> the dog are proligestone and MPA. Thes<strong>in</strong>gle subcutaneous <strong>in</strong>jection dosage recommended byLH (µg/l)FSH (µg/l)12010080604020050403020100Before 2 5 8 11Months of treatmentBefore 2 5 8 11Months of treatmentFig. 2. Plasma LH and FSH responses (mean ± SEM) <strong>in</strong> five dogs <strong>in</strong>a comb<strong>in</strong>ed anterior pituitary function test accord<strong>in</strong>g to Meij et al.(1996) before and subsequently 2, 5, 8 and 11 months after the start ofthe treatment with MPA (10 lg ⁄ kg, every 4 weeks). Blood sampleswere collected at -15, 0, 5, 10, 20, 30 and 45 m<strong>in</strong> follow<strong>in</strong>g the <strong>in</strong>jectionof the releas<strong>in</strong>g hormones at 0 m<strong>in</strong> (arrow) (Beijer<strong>in</strong>k et al. 2007)Ó 2008 The Authors. Journal compilation Ó 2008 Blackwell Verlag