Health Risks of Ionizing Radiation: - Clark University
Health Risks of Ionizing Radiation: - Clark University
Health Risks of Ionizing Radiation: - Clark University
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
174 Discussion<br />
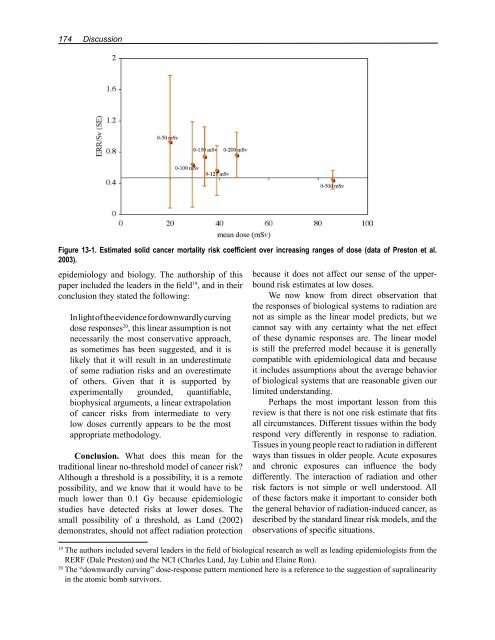
Figure 13-1. Estimated solid cancer mortality risk coefficient over increasing ranges <strong>of</strong> dose (data <strong>of</strong> Preston et al.<br />
2003).<br />
epidemiology and biology. The authorship <strong>of</strong> this<br />
paper included the leaders in the field 19 , and in their<br />
conclusion they stated the following:<br />
In light <strong>of</strong> the evidence for downwardly curving<br />
dose responses 20 , this linear assumption is not<br />
necessarily the most conservative approach,<br />
as sometimes has been suggested, and it is<br />
likely that it will result in an underestimate<br />
<strong>of</strong> some radiation risks and an overestimate<br />
<strong>of</strong> others. Given that it is supported by<br />
experimentally grounded, quantifiable,<br />
biophysical arguments, a linear extrapolation<br />
<strong>of</strong> cancer risks from intermediate to very<br />
low doses currently appears to be the most<br />
appropriate methodology.<br />
Conclusion. What does this mean for the<br />
traditional linear no-threshold model <strong>of</strong> cancer risk?<br />
Although a threshold is a possibility, it is a remote<br />
possibility, and we know that it would have to be<br />
much lower than 0.1 Gy because epidemiologic<br />
studies have detected risks at lower doses. The<br />
small possibility <strong>of</strong> a threshold, as Land (2002)<br />
demonstrates, should not affect radiation protection<br />
because it does not affect our sense <strong>of</strong> the upperbound<br />
risk estimates at low doses.<br />
We now know from direct observation that<br />
the responses <strong>of</strong> biological systems to radiation are<br />
not as simple as the linear model predicts, but we<br />
cannot say with any certainty what the net effect<br />
<strong>of</strong> these dynamic responses are. The linear model<br />
is still the preferred model because it is generally<br />
compatible with epidemiological data and because<br />
it includes assumptions about the average behavior<br />
<strong>of</strong> biological systems that are reasonable given our<br />
limited understanding.<br />
Perhaps the most important lesson from this<br />
review is that there is not one risk estimate that fits<br />
all circumstances. Different tissues within the body<br />
respond very differently in response to radiation.<br />
Tissues in young people react to radiation in different<br />
ways than tissues in older people. Acute exposures<br />
and chronic exposures can influence the body<br />
differently. The interaction <strong>of</strong> radiation and other<br />
risk factors is not simple or well understood. All<br />
<strong>of</strong> these factors make it important to consider both<br />
the general behavior <strong>of</strong> radiation-induced cancer, as<br />
described by the standard linear risk models, and the<br />
observations <strong>of</strong> specific situations.<br />
19 The authors included several leaders in the field <strong>of</strong> biological research as well as leading epidemiologists from the<br />
RERF (Dale Preston) and the NCI (Charles Land, Jay Lubin and Elaine Ron).<br />
20 The “downwardly curving” dose-response pattern mentioned here is a reference to the suggestion <strong>of</strong> supralinearity<br />
in the atomic bomb survivors.