Health Risks of Ionizing Radiation: - Clark University
Health Risks of Ionizing Radiation: - Clark University
Health Risks of Ionizing Radiation: - Clark University
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
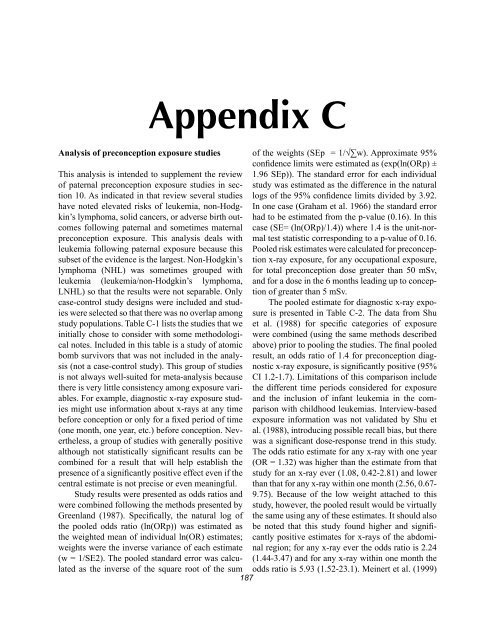
Analysis <strong>of</strong> preconception exposure studies<br />
Appendix C<br />
This analysis is intended to supplement the review<br />
<strong>of</strong> paternal preconception exposure studies in section<br />
10. As indicated in that review several studies<br />
have noted elevated risks <strong>of</strong> leukemia, non-Hodgkin’s<br />
lymphoma, solid cancers, or adverse birth outcomes<br />
following paternal and sometimes maternal<br />
preconception exposure. This analysis deals with<br />
leukemia following paternal exposure because this<br />
subset <strong>of</strong> the evidence is the largest. Non-Hodgkin’s<br />
lymphoma (NHL) was sometimes grouped with<br />
leukemia (leukemia/non-Hodgkin’s lymphoma,<br />
LNHL) so that the results were not separable. Only<br />
case-control study designs were included and studies<br />
were selected so that there was no overlap among<br />
study populations. Table C-1 lists the studies that we<br />
initially chose to consider with some methodological<br />
notes. Included in this table is a study <strong>of</strong> atomic<br />
bomb survivors that was not included in the analysis<br />
(not a case-control study). This group <strong>of</strong> studies<br />
is not always well-suited for meta-analysis because<br />
there is very little consistency among exposure variables.<br />
For example, diagnostic x-ray exposure studies<br />
might use information about x-rays at any time<br />
before conception or only for a fixed period <strong>of</strong> time<br />
(one month, one year, etc.) before conception. Nevertheless,<br />
a group <strong>of</strong> studies with generally positive<br />
although not statistically significant results can be<br />
combined for a result that will help establish the<br />
presence <strong>of</strong> a significantly positive effect even if the<br />
central estimate is not precise or even meaningful.<br />
Study results were presented as odds ratios and<br />
were combined following the methods presented by<br />
Greenland (1987). Specifically, the natural log <strong>of</strong><br />
the pooled odds ratio (ln(ORp)) was estimated as<br />
the weighted mean <strong>of</strong> individual ln(OR) estimates;<br />
weights were the inverse variance <strong>of</strong> each estimate<br />
(w = 1/SE2). The pooled standard error was calculated<br />
as the inverse <strong>of</strong> the square root <strong>of</strong> the sum<br />
187<br />
<strong>of</strong> the weights (SEp = 1/√∑w). Approximate 95%<br />
confidence limits were estimated as (exp(ln(ORp) ±<br />
1.96 SEp)). The standard error for each individual<br />
study was estimated as the difference in the natural<br />
logs <strong>of</strong> the 95% confidence limits divided by 3.92.<br />
In one case (Graham et al. 1966) the standard error<br />
had to be estimated from the p-value (0.16). In this<br />
case (SE= (ln(ORp)/1.4)) where 1.4 is the unit-normal<br />
test statistic corresponding to a p-value <strong>of</strong> 0.16.<br />
Pooled risk estimates were calculated for preconception<br />
x-ray exposure, for any occupational exposure,<br />
for total preconception dose greater than 50 mSv,<br />
and for a dose in the 6 months leading up to conception<br />
<strong>of</strong> greater than 5 mSv.<br />
The pooled estimate for diagnostic x-ray exposure<br />
is presented in Table C-2. The data from Shu<br />
et al. (1988) for specific categories <strong>of</strong> exposure<br />
were combined (using the same methods described<br />
above) prior to pooling the studies. The final pooled<br />
result, an odds ratio <strong>of</strong> 1.4 for preconception diagnostic<br />
x-ray exposure, is significantly positive (95%<br />
CI 1.2-1.7). Limitations <strong>of</strong> this comparison include<br />
the different time periods considered for exposure<br />
and the inclusion <strong>of</strong> infant leukemia in the comparison<br />
with childhood leukemias. Interview-based<br />
exposure information was not validated by Shu et<br />
al. (1988), introducing possible recall bias, but there<br />
was a significant dose-response trend in this study.<br />
The odds ratio estimate for any x-ray with one year<br />
(OR = 1.32) was higher than the estimate from that<br />
study for an x-ray ever (1.08, 0.42-2.81) and lower<br />
than that for any x-ray within one month (2.56, 0.67-<br />
9.75). Because <strong>of</strong> the low weight attached to this<br />
study, however, the pooled result would be virtually<br />
the same using any <strong>of</strong> these estimates. It should also<br />
be noted that this study found higher and significantly<br />
positive estimates for x-rays <strong>of</strong> the abdominal<br />
region; for any x-ray ever the odds ratio is 2.24<br />
(1.44-3.47) and for any x-ray within one month the<br />
odds ratio is 5.93 (1.52-23.1). Meinert et al. (1999)