- Page 3 and 4:
Abstracts - Thursday, 16 February B
- Page 5 and 6:
History of Ophthalmology 2 ........
- Page 7 and 8:
Clinicopathological Correlation: Re
- Page 9 and 10:
Basic: Intraocular Pressure in Clin
- Page 11 and 12:
Congenital and Pediatric Cataracts
- Page 13 and 14:
Free Paper: Glaucoma Thu 16 Feb 9:0
- Page 15 and 16:
FP-GLA-TH 07 (9) Phacoemulsificatio
- Page 17 and 18:
FP-REF-TH 08 (7) Ectasia Risk Score
- Page 19 and 20:
FP-RET-TH 09 (4) Ranibizumab in Age
- Page 21 and 22:
FP-PED-TH 10 (2) Multifocal Electro
- Page 23 and 24:
FP-PED-TH 10 (10) Unilateral Amblyo
- Page 25 and 26:
FP-OCP-TH 11 (8) Transcanalicular E
- Page 27 and 28:
FP-CAT-TH 12 (6) Radiofrequency Dia
- Page 29 and 30:
FP-RET-TH 13 (4) Outcome of Penetra
- Page 31 and 32:
Intermediate Thu 16 Feb 13:00 - 14:
- Page 33 and 34:
IS-RET-TH 16 (2) Polypoidal Choroid
- Page 35 and 36:
IS-CAT-TH 19 (6) Phaco Post Intacs,
- Page 37 and 38:
FP-GLA-TH 20 (9) The Electroretinog
- Page 39 and 40:
FP-REF-TH 21 (8) Outcomes of Angle-
- Page 41 and 42:
FP-RET-TH 22 (5) Advantages of Subt
- Page 43 and 44:
FP-PED-TH 23 (4) Primary Congenital
- Page 45 and 46:
IS-SOS-TH 24 (2) Pupils Bosely Thom
- Page 47 and 48:
FP-OCP-TH 25 (9) Bilateral Ritual E
- Page 49 and 50:
FP-CAT-TH 26 (8) Objective Measurem
- Page 51 and 52:
FP-RET-TH 27 (6) Imaging Retinal Pi
- Page 53 and 54:
High Refractive Errors: What Is Wor
- Page 55 and 56:
IS-PED-TH 31 (4) Education Signific
- Page 57 and 58:
IS-CAT-TH 33 (20) IOL Exchange for
- Page 59 and 60:
FP-GLA-TH 34 (10) Comparison of ICa
- Page 61 and 62:
FP-REF-TH 35 (9) Orbscan as a Prere
- Page 63 and 64:
FP-RET-TH 36 (7) Continuous Monthly
- Page 65 and 66:
FP-PED-TH 37 (4) Long Term Visual O
- Page 67 and 68:
Free Paper: Oculoplastics, Lacrimal
- Page 69 and 70:
FP-OCP-TH 39 (9) In Vivo Efficacy o
- Page 71 and 72:
FP-CAT-TH 40 (9) First Results Afte
- Page 73 and 74:
FP-RET-TH 41 (6) Outcomes of Epiret
- Page 75 and 76:
IS-REF-TH 43 (2) Scheimpflug-based
- Page 77 and 78:
IS-OCP-TH 46 (2) Enucleation in the
- Page 79 and 80:
FP-GLA-TH 48 (4) Comparison Between
- Page 81 and 82:
Free Paper: Refractive Surgery Thu
- Page 83 and 84:
FP-REF-TH 49 (9) Intraoperative Pre
- Page 85 and 86:
FP-RET-TH 50 (6) A Study on the Pre
- Page 87 and 88:
FP-PED-TH 51 (7) Acute Retinal Necr
- Page 89 and 90:
FP-CAT-TH 52 (5) Visual Outcome Aft
- Page 91 and 92:
FP-OCP-TH 53 (5) Solitary Fibrous T
- Page 93 and 94:
FP-CAT-TH 54 (5) Advantages of Usin
- Page 95 and 96:
FP-RET-TH 55 (5) Correlation of Spe
- Page 97 and 98:
Abstracts Friday 17 February
- Page 99 and 100:
IS-GLA-FR 57 (3) Canaloplasty Gries
- Page 101 and 102:
FP-RET-FR 60 (2) Ocular Primary Bla
- Page 103 and 104:
FP-RET-FR 60 (10) The Effect of Com
- Page 105 and 106:
IS-STR-FR 63 (2) Dysthyroid Myopath
- Page 107 and 108:
Free Paper: Pathology Fri 17 Feb 8:
- Page 109 and 110:
FP-PAT-FR 66 (10) Relative Contribu
- Page 111 and 112:
Epidemiology of Uveitis and Related
- Page 113 and 114:
FP-REF-FR 71 (8) Management of Extr
- Page 115 and 116:
FP-COR-FR 72 (5) CFTR is Functional
- Page 117 and 118:
FP-ONC-FR 73 (5) Criteria for Posto
- Page 119 and 120:
FP-CAT-FR 74 (2) Anticardiolipin An
- Page 121 and 122:
Trabectome Surgery for Infantile Gl
- Page 123 and 124:
Keratoconus and Ectatic Disorders:
- Page 125 and 126:
The Hot Orbit Fri 17 Feb 10:30 - 12
- Page 127 and 128:
IS-ONC-FR 89 (3) Adjuvant Therapy i
- Page 129 and 130:
Contact Lenses 2 Fri 17 Feb 10:30 -
- Page 131 and 132:
IS-PER-FR 96 (5) Secondary Glaucoma
- Page 133 and 134:
FP-COR-FR 97 (8) Saving Sight in Co
- Page 135 and 136:
FP-RET-FR 98 (5) Intravitreal (IVT)
- Page 137 and 138:
FP-PHA-FR 99 (2) A New Therapeutic
- Page 139 and 140:
Difficult Situations in Phacoemulsi
- Page 141 and 142:
Current Trends in Corneal Replaceme
- Page 143 and 144:
IS-OCP-FR 110 (2) Synkinetic Ptosis
- Page 145 and 146:
IS-ONC-FR 113 (3) Emerging Molecula
- Page 147 and 148:
IS-WFS-FR 116 (4) Report from the A
- Page 149 and 150:
Free Paper: Strabismus Fri 17 Feb 1
- Page 151 and 152:
FP-STR-FR 121 (9) Adjustable Squint
- Page 153 and 154:
FP-RET-FR 122 (7) Intravitreal Beva
- Page 155 and 156:
FP-CAT-FR 123 (4) Patient Satisfact
- Page 157 and 158:
Strategies for Very Dense Nuclei an
- Page 159 and 160:
IS-VID-FR 130 (2) Phaco-trabeculect
- Page 161 and 162:
IS-RET-FR 133 (5) Choroidal Surgery
- Page 163 and 164:
IS-CAT-FR 136 (3) Difractive vs. Re
- Page 165 and 166:
IS-TEC-FR 139 (2) Future Therapeuti
- Page 167 and 168:
IS-SOS-FR 142 (2) When to Refer the
- Page 169 and 170:
Free Paper: External Eye Disease, C
- Page 171 and 172:
FP-COR-FR 146 (10) Repeatability an
- Page 173 and 174:
FP-RET-FR 147 (7) Sutureless 23 G V
- Page 175 and 176:
FP-UVE-FR 148 (4) Clinical Patterns
- Page 177 and 178:
Strategies for Very Dense Nuclei an
- Page 179 and 180:
Abstracts Saturday 18 February
- Page 181 and 182:
IS-TRA-SA 158 (2) Pearls and Pitfal
- Page 183 and 184:
IS-CAT-SA 161 (2) Cataract Surgery
- Page 185 and 186:
Assessment of Clinical Skills of Re
- Page 187 and 188:
IS-EVI-SA 168 (4) Summary of Eviden
- Page 189 and 190:
FP-PED-SA 171 (4) Optical Iridectom
- Page 191 and 192:
FP-ONC-SA 172 (3) Conjunctival Squa
- Page 193 and 194:
FP-CAT-SA 173 (2) The Visual and Re
- Page 195 and 196:
How to Write a Scientific Paper Sat
- Page 197 and 198:
Novel Mechanisms and Risk Factors f
- Page 199 and 200:
IS-RET-SA 183 (6) Intravascular Thr
- Page 201 and 202:
IS-CAT-SA 186 (5) Management of Mul
- Page 203 and 204:
Epidemiology of Childhood Blindness
- Page 205 and 206:
IS-SOS-SA 192 (6) Dyslexia Alkhudai
- Page 207 and 208:
Free Paper: External Eye Disease, C
- Page 209 and 210:
FP-COR-SA 196 (9) Study of Nomogram
- Page 211 and 212:
FP-RET-SA 197 (8) RaScaL Study: A N
- Page 213 and 214:
FP-CAT-SA 198 (5) Unilateral Diffra
- Page 215 and 216:
Pediatric Cataract Surgery: Conquer
- Page 217 and 218:
IS-GLA-SA 205 (7) Glaucoma and Opti
- Page 219 and 220:
Age-Related Macular Degeneration an
- Page 221 and 222:
IS-REF-SA 210 (5) Results of Lamell
- Page 223 and 224:
Computer-Aided Diagnosis, Novel Ima
- Page 225 and 226:
IS-LOW-SA 215 (4) Bitemporal Hemian
- Page 227 and 228:
IC-SCS-SA 219 (4) I›ll Accept thi
- Page 229 and 230:
FP-COR-SA 220 (9) Effect of Corneal
- Page 231 and 232:
FP-EPI-SA 221 (7) The Cost-Effectiv
- Page 233 and 234:
FP-CAT-SA 222 (5) The Results of To
- Page 235 and 236:
IS-SSS-SA 229 (4) Inequality of Tra
- Page 237 and 238:
Age-Related Macular Degeneration: N
- Page 239 and 240:
IS-NEO-SA 235 (4) Automated Static
- Page 241 and 242:
IS-EDU-SA 238 (2) A Checklist of St
- Page 243 and 244:
IS-EVI-SA 241 (6) Glaucoma Eye Drop
- Page 245 and 246:
FP-IMG-SA 243 (9) Usefulness of Ang
- Page 247 and 248:
FP-COR-SA 244 (10) Immunocytochemic
- Page 249 and 250:
FP-RET-SA 245 (11) Two-photon Excit
- Page 251 and 252:
What Will You Do? Sat 18 Feb 15:30
- Page 253 and 254:
Abstracts Sunday 19 February
- Page 255 and 256:
IS-GLA-SU 253 (4) Efficacy of Ologe
- Page 257 and 258:
Retina Hot Topics Sun 19 Feb 8:30 -
- Page 259 and 260:
FP-OCP-SU 257 (6) Eyelid Retraction
- Page 261 and 262:
Free Paper: Oncology Sun 19 Feb 8:3
- Page 263 and 264:
FP-ONC-SU 260 (11) Effect of Intrav
- Page 265 and 266:
IS-WFS-SU 263 (4) How Can we Increa
- Page 267 and 268:
IS-UVE-SU 266 (4) Glaucoma Surgery
- Page 269 and 270:
FP-COR-SU 268 (6) Intrastromal Amph
- Page 271 and 272:
FP-TRA-SU 269 (4) The role of Amylo
- Page 273 and 274:
FP-REF-SU 270 (2) Refractive and Ab
- Page 275 and 276:
FP-REF-SU 270 (11) Outcome of Simul
- Page 277 and 278:
Wound Management and Bleb Problems
- Page 279 and 280:
IS-RET-SU 281 (5) Beneficial of Dir
- Page 281 and 282:
IS-STR-SU 284 (3) Genetics and Chil
- Page 283 and 284:
IS-ONC-SU 285 (19) Orbit: 17 Year O
- Page 285 and 286:
IS-WFS-SU 288 (6) Residency Program
- Page 287 and 288:
FP-CLR-SU 290 (5) Heritability of P
- Page 289 and 290:
IS-SCS-SU 292 (4) Minimally Invasiv
- Page 291 and 292:
FP-COR-SU 293 (8) Three-Year Result
- Page 293 and 294:
FP-RET-SU 294 (6) Clinical and Opti
- Page 295 and 296:
FP-OCP-SU 295 (4) Long term follow-
- Page 297 and 298:
Corneal Specular Microscopy Sun 19
- Page 299 and 300:
New Therapeutic Approaches in Glauc
- Page 301 and 302:
Diagnosis and Management of Retinop
- Page 303 and 304:
IS-REF-SU 308 (10) Is Pseudophakia
- Page 305 and 306:
IS-TEC-SU 311 (6) New Developments
- Page 307 and 308:
IS-CLR-SU 315 (3) The Oliver Dabezi
- Page 309 and 310:
FP-IMG-SU 317 (6) Nonmy Driatic Scr
- Page 311 and 312:
FP-COR-SU 318 (3) Collagen Crosslin
- Page 313 and 314:
FP-COR-SU 318 (11) Evidence of Impr
- Page 315 and 316:
FP-WFS-SU 319 (8) Cataract Surgery
- Page 317 and 318:
FP-CAT-SU 320 (5) Refractive Predic
- Page 319 and 320:
FR-CAT-SU 325 (8) Implants Phaques
- Page 321 and 322:
Cornea and Eye Banking in India Sun
- Page 323 and 324:
Complex and Difficult Management De
- Page 325 and 326:
Prognostic Biopsy of Uveal Melanoma
- Page 327 and 328:
IS-WFS-SU 337 (3) The Role of Natio
- Page 329 and 330:
IS-PHA-SU 340 (3) Managing the Infl
- Page 331 and 332:
FP-HIS-SU 341 (7) Supporting an Eme
- Page 333 and 334:
FP-COR-SU 342 (5) Efficacy of Intac
- Page 335 and 336:
FP-ONC-SU 343 (2) Large Basal Cell
- Page 337 and 338:
Free Paper: Refractive Surgery Sun
- Page 339 and 340:
Using Computers for Managing Patien
- Page 341 and 342:
Abstracts Monday 20 February
- Page 343 and 344:
IS-GLA-MO 352 (3) What Tests are Mo
- Page 345 and 346:
IS-RET-MO 354 (3) Summary of DRCR.n
- Page 347 and 348:
IS-OCP-MO 356 (5) Refining the Outc
- Page 349 and 350:
FP-REF-MO 357 (10) Using Objective
- Page 351 and 352:
IS-TEC-MO 360 (6) Signaling Pathway
- Page 353 and 354:
IS-STR-MO 363 (6) Adaptive Optics i
- Page 355 and 356:
FP-WFS-MO 366 (3) Compliance of Spe
- Page 357 and 358:
Free Paper: External Eye Disease, C
- Page 359 and 360:
FP-COR-MO 367 (10) Toxic Epidermal
- Page 361 and 362:
FP-TRA-MO 368 (8) Prospective Study
- Page 363 and 364:
FP-CAT-MO 369 (5) Outcomes After Cr
- Page 365 and 366:
Education Without Borders: The Futu
- Page 367 and 368:
FP-GLA-MO 374 (6) Survey of Glaucom
- Page 369 and 370:
IS-COR-MO 376 (2) Endothelial Cell
- Page 371 and 372:
FP-TRA-MO 377 (5) Assessment of Fac
- Page 373 and 374:
FP-RET-MO 378 (2) A Detailed Evalua
- Page 375 and 376:
FP-RET-MO 378 (10) Correlation Betw
- Page 377 and 378:
Free Paper: Strabismus Mon 20 Feb 1
- Page 379 and 380:
FP-STR-MO 381 (9) Immediate Post-Op
- Page 381 and 382:
IS-PAT-MO 383 Clinicopathological C
- Page 383 and 384:
FP-EPI-MO 384 (9) Eye Care Programm
- Page 385 and 386:
FP-NEO-MO 386 (5) Toxoplasma Neuror
- Page 387 and 388:
Contact Lens - Newton Kara José Sy
- Page 389 and 390:
FP-COR-MO 389 (4) Calcium Channels
- Page 391 and 392:
FP-EPI-MO 390 (2) The Distribution
- Page 393 and 394:
FP-EPI-MO 390 (10) Optical Quality
- Page 395 and 396:
FP-OCP-MO 391 (8) Fat Transfer for
- Page 397 and 398:
Free Paper: Retina - Medical Mon 20
- Page 399 and 400:
FP-RET-MO 396 (9) Results of the Ph
- Page 401 and 402:
FP-GLA-MO 397 (8) A New Approach fo
- Page 403 and 404:
FP-COR-MO 398 (5) Visual Results of
- Page 405 and 406:
FP-TRA-MO 399 (3) Role of Ophthalmi
- Page 407 and 408:
FP-REF-MO 400 (3) Using a Small Ape
- Page 409 and 410:
FP-REF-MO 400 (11) The KAMRA Intrac
- Page 411 and 412:
FP-OCP-MO 401 (9) To Describe a Nov
- Page 413 and 414:
FP-CAT-MO 402 (7) Three-Port MICS (
- Page 415 and 416:
Free Paper: Oncology Mon 20 Feb 13:
- Page 417 and 418:
FP-ONC-MO 404 (9) Plaque Therapy fo
- Page 419 and 420:
FP-TEC-MO 405 (6) Teleophthalmology
- Page 421 and 422:
FP-EPI-MO 406 (4) Prevalence and As
- Page 423 and 424:
Free Paper: Prevention of Blindness
- Page 425 and 426:
FP-WFS-MO 407 (9) RAAB Surveys: A T
- Page 427 and 428:
FP-EDU-MO 408 (6) Effect of Univers
- Page 429 and 430:
FP-IMM-MO 409 (3) TNF- a and Glycat
- Page 431 and 432:
FP-IMM-MO 409 (11) Th1/Th2 Cytokine
- Page 433 and 434:
FP-UVE-MO 410 (8) Ocular Features i
- Page 435 and 436:
FP-COR-MO 411 (5) Tunnel Infection
- Page 437 and 438:
FP-STR-MO 412 (3) A Relationship be
- Page 439 and 440:
Workshop on e-Learning Tools Mon 20
- Page 441 and 442:
Video Cataract VI-CAT-01 Alice in V
- Page 443 and 444:
I-CAT-16 Microincisional Surgery of
- Page 445 and 446:
VI-CAT-30 CATARACT SURGERY ‹REVOL
- Page 447 and 448:
VI-CAT-48 A NEW PHACO NEEDLE Joseph
- Page 449 and 450:
VI-CAT-62 Challenges in Intraocular
- Page 451 and 452:
VI-CAT-76 Primary Posterior Capsulo
- Page 453 and 454:
VI-COR-14 A video demonstrating ret
- Page 455 and 456:
Ophthalmic Education VI-EDU-01 Lase
- Page 457 and 458:
VI-GLA-12 Combined cataract and Gla
- Page 459 and 460:
Low Vision and Rehabilitation VI-LO
- Page 461 and 462:
VI-OCP-11 Lateral tarsal STRIP Unde
- Page 463 and 464:
Oncology VI-ONC-01 Ocular Surface S
- Page 465 and 466:
Refractive Surgery VI-REF-01 Persis
- Page 467 and 468:
VI-RET-10 Is process of epiretinal
- Page 469 and 470:
VI-RET-26 Nanophthalmic uveal effus
- Page 471 and 472:
Eye Trauma and Emergencies VI-TRA-0
- Page 473 and 474:
PO-CAT-06 Outcomes of Unilatteral T
- Page 475 and 476:
PO-CAT-15 Cataract Surgery Outcome
- Page 477 and 478:
PO-CAT-26 Piggy Back ioil Implantat
- Page 479 and 480:
PO-CAT-34 The Results of OZIL IP So
- Page 481 and 482:
PO-CAT-43 Influence of Emoxipin on
- Page 483 and 484:
PO-CAT-52 Vector Analysis of Astigm
- Page 485 and 486:
PO-CAT-62 Akreos Adapt Calcificatio
- Page 487 and 488:
PO-CAT-71 A New Era in Manual SICS
- Page 489 and 490:
PO-CAT-79 The New Helical Composite
- Page 491 and 492:
PO-CLR-04 Therapeutic Use of Fluoro
- Page 493 and 494:
Evidence Based Ophthalmology PO-EVI
- Page 495 and 496:
PO-COR-8 Corneal Microsporidiosis S
- Page 497 and 498:
PO-COR-17 Documentation of Keratoco
- Page 499 and 500:
PO-COR-26 Corneal Collagen Crosslin
- Page 501 and 502:
PO-COR-34 Results of Descemets Stri
- Page 503 and 504:
PO-COR-44 Comparison of Rose Bengal
- Page 505 and 506:
PO-COR-54 Corneal Cross-Linking as
- Page 507 and 508:
PO-COR-65 Tpical tacrolimus as a tr
- Page 509 and 510:
PO-COR-74 Extensive bilateral corne
- Page 511 and 512:
PO-COR-85 Short Term Visual Outcome
- Page 513 and 514:
PO-COR-94 Successful treatment of f
- Page 515 and 516:
PO-COR-103 Descemet´s membrane det
- Page 517 and 518:
PO-COR-114 ANATOMICAL AND FUNCTIONA
- Page 519 and 520:
PO-COR-122 Post-keratoplasty emerge
- Page 521 and 522:
PO-COR-130 Fungal keratitis: a UKMM
- Page 523 and 524:
PO-TRA-08 Epidemiology of Canalicul
- Page 525 and 526:
PO-TRA-19 An infant case of traumat
- Page 527 and 528:
PO-GLA-07 Comparison of Optic Nerve
- Page 529 and 530:
PO-GLA-15 Novel, minimally invasive
- Page 531 and 532:
PO-GLA-23 Evaluation Of Surgical Tr
- Page 533 and 534:
PO-GLA-31 Epidemiology of Clinical
- Page 535 and 536:
PO-GLA-40 Family history a vital ri
- Page 537 and 538:
PO-GLA-50 The Measurement of the In
- Page 539 and 540:
PO-GLA-60 EMERGING PATTERNS AND FAC
- Page 541 and 542:
PO-GLA-69 Angle closure glaucoma in
- Page 543 and 544:
PO-GLA-78 Efficacy of needling with
- Page 545 and 546:
PO-IMM-02 Symptomatic behavior of c
- Page 547 and 548:
PO-IMM-13 Identification of Autoant
- Page 549 and 550:
Low Vision and Rehabilitation PO-LO
- Page 551 and 552:
PO-NEO-06 Familial occurrence of op
- Page 553 and 554:
PO-NEO-18 Myastenia Gravis: 2 Cases
- Page 555 and 556:
PO-TEC-05 Polyurethane biodegradabl
- Page 557 and 558:
PO-IMG-04 EVALUATION OF TEAR FILM Q
- Page 559 and 560:
PO-IMG-13 A Prospective Study to Ac
- Page 561 and 562:
PO-IMG-22 Biometry of the anterior
- Page 563 and 564:
PO-OCP-10 Basics of external dacryo
- Page 565 and 566:
PO-OCP-19 Surgical Outcomes of Pedi
- Page 567 and 568:
PO-OCP-27 Morphological changes of
- Page 569 and 570:
PO-OCP-38 Demographic of Patients w
- Page 571 and 572:
PO-OCP-48 Acquired severe contracte
- Page 573 and 574:
PO-OCP-58 effectiveness of silicone
- Page 575 and 576:
PO-OCP-68 ANOPHTALMIA -ABOUT three
- Page 577 and 578:
PO-ONC-06 Clinical Profile, Managem
- Page 579 and 580:
PO-ONC-15 Use of Mitomycin-C and In
- Page 581 and 582:
PO-ONC-23 CONJUNCTIVAL TUMORS(about
- Page 583 and 584:
PO-ONC-33 Orbital Recurrence follow
- Page 585 and 586:
Ophthalmic Epidemiology PO-EPI-01 P
- Page 587 and 588:
PO-EPI-11 Tear Function in an Irani
- Page 589 and 590:
PO-EPI-19 The Annual Direct Cost of
- Page 591 and 592:
PO-PAT-02 EFFECTS OF X RADIATION ON
- Page 593 and 594:
PO-PED-06 A novel phenotype of juve
- Page 595 and 596:
PO-PED-16 Retinoblastoma Masqueradi
- Page 597 and 598:
PO-PED-26 Prevalence of RDS periphe
- Page 599 and 600:
PO-PED-35 Managing Peadiatric Catar
- Page 601 and 602:
PO-WFS-03 Prevalence and causes of
- Page 603 and 604: PO-WFS-13 Surgical Expedition to Gh
- Page 605 and 606: PO-REF-06 Improving the predictabil
- Page 607 and 608: PO-REF-16 Refractive and Optical Qu
- Page 609 and 610: PO-REF-25 Nodular Episcleritis afte
- Page 611 and 612: PO-REF-35 Comparative electron micr
- Page 613 and 614: PO-RET-04 Examining Recalcitrant Di
- Page 615 and 616: PO-RET-13 Sterile Endophthalmitis a
- Page 617 and 618: PO-RET-21 Diagnostic and Management
- Page 619 and 620: PO-RET-30 Red blood cell targeted c
- Page 621 and 622: PO-RET-40 Is Fundus fluorescein ang
- Page 623 and 624: PO-RET-49 Isotretinoin associated t
- Page 625 and 626: PO-RET-61 The outcome of intravitre
- Page 627 and 628: PO-RET-70 TRAINING AND ACCREDITATIO
- Page 629 and 630: PO-RET-79 Valsalva Retinopathy duri
- Page 631 and 632: PO-RET-89 Hypoxia-inducible factor-
- Page 633 and 634: PO-RET-98 BRAO - It is never too la
- Page 635 and 636: PO-RET-106 Retinal Manifestations o
- Page 637 and 638: PO-RET-116 Camp Approach to Diabeti
- Page 639 and 640: PO-RET-125 Idiopathic Macular Telan
- Page 641 and 642: PO-RET-134 Acute Retinal Necrosis A
- Page 643 and 644: PO-RET-144 Scleral Buckling Surgery
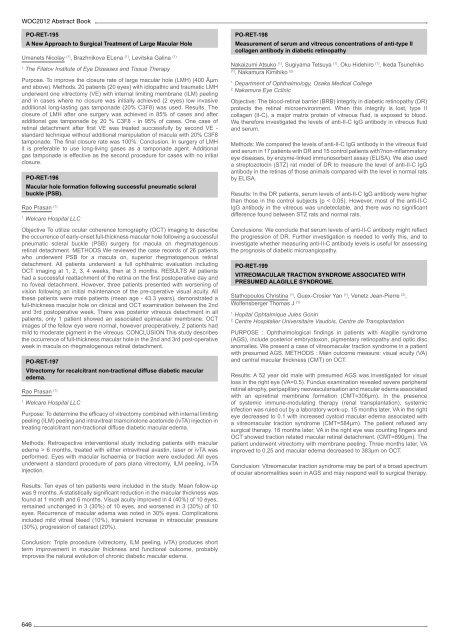
- Page 645 and 646: PO-RET-152 Comparison of internal l
- Page 647 and 648: PO-RET-161 Optical coherence tomogr
- Page 649 and 650: PO-RET-171 Management of recurrent
- Page 651 and 652: PO-RET-180 Visual and surgical outc
- Page 653: PO-RET-190 Pediatric Vitrectomy in
- Page 657 and 658: Strabismus PO-STR-01 Evaluation of
- Page 659 and 660: PO-STR-12 Congenital Superior Obliq
- Page 661 and 662: PO-STR-23 Quality of Life and Cost-
- Page 663 and 664: PO-UVE-03 Recurrence of presumed bi
- Page 665 and 666: PO-UVE-12 SIL2R, Neopterin and angi
- Page 667 and 668: PO-UVE-23 Clinical features of pati
- Page 669 and 670: PO-UVE-32 Ocular tuberculoma with a
- Page 671 and 672: Akbarzadeh Siamak : 164 Akcetin Tul
- Page 673 and 674: Ansari Astaneh mohammad reza : 555
- Page 675 and 676: Bi Xiaoping : 61 Bialasiewicz Alexa
- Page 677 and 678: Constable Ian : 177 Constable Ian :
- Page 679 and 680: El-Sebaity Dalia M : 236 Elserogy H
- Page 681 and 682: Goes Frank : 186 Gogate Parikshit :
- Page 683 and 684: Honavar Santosh : 38, 98, 110, 117,
- Page 685 and 686: Kaminska Anna : 395, 474 Kamlesh :
- Page 687 and 688: Kumar Mahesh : 376 Kumar Najith : 6
- Page 689 and 690: Markuszewska Anna : 600 Markuszewsk
- Page 691 and 692: Myint Kay Thi : 417 Myrowitz Elliot
- Page 693 and 694: Pang Calvin : 118, 211 Pangarkar An
- Page 695 and 696: Reddy J. K. : 181 Reddy Jagadesh :
- Page 697 and 698: Shaarawy Ashraf : 86, 207, 239 Shaa
- Page 699 and 700: Sullivan Paul : 22, 66 Sullivan Tim
- Page 701 and 702: Vetrugno Michele : 88 Victoria Dari