Annual Meeting Proceedings Part 1 - American Society of Clinical ...
Annual Meeting Proceedings Part 1 - American Society of Clinical ...
Annual Meeting Proceedings Part 1 - American Society of Clinical ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
130s Central Nervous System Tumors<br />
2060 General Poster Session (Board #14G), Sat, 1:15 PM-5:15 PM<br />
Tolerance and feasibility <strong>of</strong> chemotherapy by procarbazine, lomustine, and<br />
vincristine (PCV) for oligodendroglial anaplastic gliomas (OAG). Presenting<br />
Author: Marine Davos, University Hospital Timone, Marseille, France<br />
Background: Chemosensitivity <strong>of</strong> OAG has been documented although their<br />
role as part <strong>of</strong> adjuvant treatment combined to radiotherapy is debated.<br />
Beside temozolomide still under investigation, several studies have underlined<br />
activity <strong>of</strong> PCV regimen in this setting. However, significant toxicity<br />
has been described and dose intensity and schedule duration are not<br />
clearly reported. Methods: This monocentric retrospective analysis included<br />
all pts with OAG treated with at least 1 cycle <strong>of</strong> PVC (lomustine 110mg/m2<br />
every 6 weeks) at our institution from August 2007 to August 2011<br />
(pharmacy charter). Toxicities data were collected from clinical observations<br />
and blood investigations. Results: 40 pts were identified (M/F: 23/17).<br />
Median age was 45y (20 – 72). At the time <strong>of</strong> analyses, 32 pts were still<br />
alive. Histologies were oligodendroglioma (73%) or oligoastrocytoma (27%).<br />
Codeletion 1p19q was observed in 30 % <strong>of</strong> pts. PCV was administered in<br />
first or second line <strong>of</strong> chemotherapy for 60 % and 40 % <strong>of</strong> pts respectively.<br />
Seventy five percent and 52.5% <strong>of</strong> pts completed at least <strong>of</strong> 4 and 6 cycles<br />
respectively. Discontinuation <strong>of</strong> PCV occurred in 45% <strong>of</strong> pts for toxicity<br />
(10%), progression (30%), or other reason (5%). Because <strong>of</strong> toxicity<br />
38/196 (19%) PCV cycles were delayed. Dose was adapted for 73% <strong>of</strong> pts<br />
and decreased under 60% <strong>of</strong> theoretical dose in 30% <strong>of</strong> pts at cycle 4 and<br />
in 57% <strong>of</strong> pts at cycle 6 (table1). Grade III or IV toxicity occurred in 28% <strong>of</strong><br />
pts and only grade I-II in 50%. Neuropathies occurred in 43 % <strong>of</strong> pts.<br />
Conclusions: Despite activity <strong>of</strong> PCV regimen, significant toxicity is associated<br />
to this schedule, that impact feasibility and compliance. PVC<br />
schedule should be redefined taking into account dose intensity applied in<br />
toxicity observed.<br />
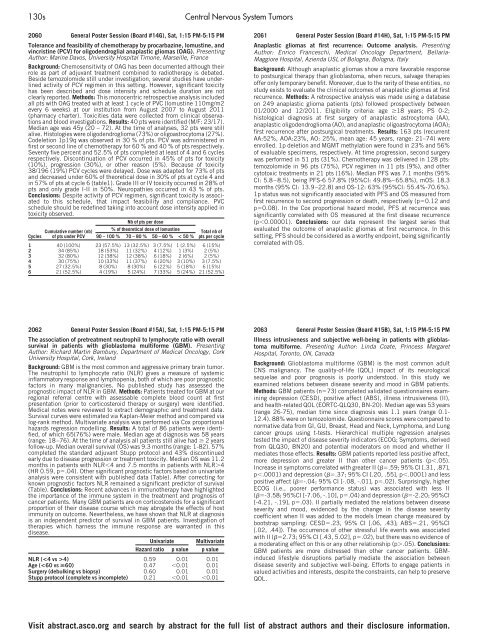
Cycles<br />
Cumulative number (nb)<br />
<strong>of</strong> pts under PCV<br />
Nb <strong>of</strong> pts per dose<br />
% <strong>of</strong> theoretical dose <strong>of</strong> lomustine<br />
90–100% 70–80% 50–60% < 50 %<br />
Total nb <strong>of</strong><br />
pts per cycle<br />
1 40 (100%) 23 (57.5%) 13 (32.5%) 3 (7.5%) 1 (2.5%) 6 (15%)<br />
2 34 (85%) 18 (53%) 11 (32%) 4 (12%) 1 (3%) 2 (5%)<br />
3 32 (80%) 12 (38%) 12 (38%) 6 (18%) 2 (6%) 2 (5%)<br />
4 30 (75%) 10 (33%) 11 (37%) 6 (20%) 3 (10%) 3 (7.5%)<br />
5 27 (32.5%) 8 (30%) 8 (30%) 6 (22%) 5 (18%) 6 (15%)<br />
6 21 (52.5%) 4 (19%) 5 (24%) 7 (33%) 5 (24%) 21 (52.5%)<br />
2062 General Poster Session (Board #15A), Sat, 1:15 PM-5:15 PM<br />
The association <strong>of</strong> pretreatment neutrophil to lymphocyte ratio with overall<br />
survival in patients with glioblastoma multiforme (GBM). Presenting<br />
Author: Richard Martin Bambury, Department <strong>of</strong> Medical Oncology, Cork<br />
University Hospital, Cork, Ireland<br />
Background: GBM is the most common and aggressive primary brain tumor.<br />
The neutrophil to lymphocyte ratio (NLR) gives a measure <strong>of</strong> systemic<br />
inflammatory response and lymphopenia, both <strong>of</strong> which are poor prognostic<br />
factors in many malignancies. No published study has assessed the<br />
prognostic impact <strong>of</strong> NLR in GBM. Methods: Patients treated for GBM at our<br />
regional referral centre with assessable complete blood count at first<br />
presentation (prior to corticosteroid therapy or surgery) were identified.<br />
Medical notes were reviewed to extract demographic and treatment data.<br />
Survival curves were estimated via Kaplan-Meier method and compared via<br />
log-rank method. Multivariate analysis was performed via Cox proportional<br />
hazards regression modelling. Results: A total <strong>of</strong> 86 patients were identified,<br />
<strong>of</strong> which 65(76%) were male. Median age at diagnosis was 58 years<br />
(range: 18–76). At the time <strong>of</strong> analysis all patients still alive had � 2 years<br />
follow-up. Median overall survival (OS) was 9.3 months (range: 1-82). 57%<br />
completed the standard adjuvant Stupp protocol and 43% discontinued<br />
early due to disease progression or treatment toxicity. Median OS was 11.2<br />
months in patients with NLR�4 and 7.5 months in patients with NLR�4<br />
(HR 0.59, p�.04). Other significant prognostic factors based on univariate<br />
analysis were consistent with published data (Table). After correcting for<br />
known prognostic factors NLR remained a significant predictor <strong>of</strong> survival<br />
(Table). Conclusions: Recent advances in immunotherapy have highlighted<br />
the importance <strong>of</strong> the immune system in the treatment and prognosis <strong>of</strong><br />
cancer patients. Many GBM patients are on corticosteroids for a significant<br />
proportion <strong>of</strong> their disease course which may abrogate the effects <strong>of</strong> host<br />
immunity on outcome. Nevertheless, we have shown that NLR at diagnosis<br />
is an independent predictor <strong>of</strong> survival in GBM patients. Investigation <strong>of</strong><br />
therapies which harness the immune response are warranted in this<br />
disease.<br />
Univariate Multivariate<br />
Hazard ratio p value p value<br />
NLR (4) 0.59 0.01 0.01<br />
Age (60) 0.47 �0.01 0.01<br />
Surgery (debulking vs biopsy) 0.60 0.01 0.01<br />
Stupp protocol (complete vs incomplete) 0.21 �0.01 �0.01<br />
2061 General Poster Session (Board #14H), Sat, 1:15 PM-5:15 PM<br />
Anaplastic gliomas at first recurrence: Outcome analysis. Presenting<br />
Author: Enrico Franceschi, Medical Oncology Department, Bellaria-<br />
Maggiore Hospital, Azienda USL <strong>of</strong> Bologna, Bologna, Italy<br />
Background: Although anaplastic gliomas show a more favorable response<br />
to postsurgical therapy than glioblastoma, when recurs, salvage therapies<br />
<strong>of</strong>fer only temporary benefit. Moreover, due to the rarity <strong>of</strong> these entities, no<br />
study exists to evaluate the clinical outcomes <strong>of</strong> anaplastic gliomas at first<br />
recurrence. Methods: A retrospective analysis was made using a database<br />
on 249 anaplastic glioma patients (pts) followed prospectively between<br />
01/2000 and 12/2011. Eligibility criteria: age �18 years; PS 0-2;<br />
histological diagnosis at first surgery <strong>of</strong> anaplastic astrocytoma (AA),<br />
anaplastic oligodendroglioma (AO), and anaplastic oligoastrocytoma (AOA);<br />
first recurrence after postsurgical treatments. Results: 163 pts (recurrent<br />
AA:52%, AOA:23%, AO: 25%, mean age: 45 years, range: 21–74) were<br />
enrolled. 1p deletion and MGMT methylation were found in 23% and 56%<br />
<strong>of</strong> evaluable specimens, respectively. At time progression, second surgery<br />
was performed in 51 pts (31%). Chemotherapy was delivered in 128 pts:<br />
temozolomide in 96 pts (75%), PCV regimen in 11 pts (9%), and other<br />
cytotoxic treatments in 21 pts (16%). Median PFS was 7.1 months (95%<br />
CI: 5.8–8.5), being PFS-6 57.8% (95%CI: 49.8%–65.8%), mOS: 18.3<br />
months (95% CI: 13.9–22.8) and OS-12: 63% (95%CI: 55.4%-70.6%).<br />
1p status was not significantly associated with PFS and OS measured from<br />
first recurrence to second progression or death, respectively (p�0.12 and<br />
p�0.08). In the Cox proportional hazard model, PFS at recurrence was<br />
significantly correlated with OS measured at the first disease recurrence<br />
(p�0.00001). Conclusions: our data represent the largest series that<br />
evaluated the outcome <strong>of</strong> anaplastic gliomas at first recurrence. In this<br />
setting, PFS should be considered as a worthy endpoint, being significantly<br />
correlated with OS.<br />
2063 General Poster Session (Board #15B), Sat, 1:15 PM-5:15 PM<br />
Illness intrusiveness and subjective well-being in patients with glioblastoma<br />
multiforme. Presenting Author: Linda Coate, Princess Margaret<br />
Hospital, Toronto, ON, Canada<br />
Background: Glioblastoma multiforme (GBM) is the most common adult<br />
CNS malignancy. The quality-<strong>of</strong>-life (QOL) impact <strong>of</strong> its neurological<br />
sequelae and poor prognosis is poorly understood. In this study we<br />
examined relations between disease severity and mood in GBM patients.<br />
Methods: GBM patients (n�73) completed validated questionnaires examining<br />
depression (CESD), positive affect (ABS), illness intrusiveness (II),<br />
and health-related QOL (EORTC-QLQ30, BN-20). Median age was 53 years<br />
(range 26-75), median time since diagnosis was 1.1 years (range 0.1-<br />
12.4). 88% were on temozolomide. Questionnaire scores were compared to<br />
normative data from GI, GU, Breast, Head and Neck, Lymphoma, and Lung<br />
cancer groups using t-tests. Hierarchical multiple regression analyses<br />
tested the impact <strong>of</strong> disease severity indicators (ECOG; Symptoms, derived<br />
from QLQ30, BN20) and potential moderators on mood and whether II<br />
mediates those effects. Results: GBM patients reported less positive affect,<br />
more depression and greater II than other cancer patients (p�.05).<br />
Increase in symptoms correlated with greater II (��.59; 95% CI [.31, .87],<br />
p�.0001) and depression (��.37; 95% CI [.20, .55], p�.0001) and less<br />
positive affect (��-.04; 95% CI [-.08, -.01], p�.02). Surprisingly, higher<br />
ECOG (i.e., poorer performance status) was associated with less II<br />
(��-3.58; 95%CI [-7.06, -.10], p�.04) and depression (��-2.20; 95%CI<br />
[-4.21, -.19], p�.03). II partially mediated the relations between disease<br />
severity and mood, evidenced by the change in the disease severity<br />
coefficient when II was added to the models (mean change measured by<br />
bootstrap sampling: CESD�.23, 95% CI [.06, .43]; ABS�.21, 95%CI<br />
[.02, .44]). The occurrence <strong>of</strong> other stressful life events was associated<br />
with II (��2.73; 95% CI [.43, 5.02], p�.02), but there was no evidence <strong>of</strong><br />
a moderating effect on this or any other relationship (p�.05). Conclusions:<br />
GBM patients are more distressed than other cancer patients. GBMinduced<br />
lifestyle disruptions partially mediate the association between<br />
disease severity and subjective well-being. Efforts to engage patients in<br />
valued activities and interests, despite the constraints, can help to preserve<br />
QOL.<br />
Visit abstract.asco.org and search by abstract for the full list <strong>of</strong> abstract authors and their disclosure information.