Annual Meeting Proceedings Part 1 - American Society of Clinical ...
Annual Meeting Proceedings Part 1 - American Society of Clinical ...
Annual Meeting Proceedings Part 1 - American Society of Clinical ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
14s Breast Cancer—HER2/ER<br />
528 Poster Discussion Session (Board #18), Sat, 1:15 PM-5:15 PM and<br />
4:45 PM-5:45 PM<br />
Results from a phase Ib study <strong>of</strong> trastuzumab emtansine (T-DM1),<br />
paclitaxel (T), and pertuzumab (P) in patients with HER2-positive metastatic<br />
breast cancer (MBC) previously treated with trastuzumab. Presenting<br />
Author: Shanu Modi, Memorial Sloan-Kettering Cancer Center, New York,<br />
NY<br />
Background: The antibody–drug conjugate T-DM1 has shown single-agent<br />
activity in phase II studies in patients (pts) with HER2–positive MBC.<br />
Preclinical data suggest synergy for T-DM1 combined with taxanes and with<br />
P. Methods: TDM4652g is a phase Ib, open-label, dose-escalation study<br />
evaluating the safety and tolerability <strong>of</strong> T-DM1 (qw and q3w) � T (qw) � P<br />
(q3w) in pts with HER2-positive MBC previously treated with trastuzumab.<br />
A3�3 dose-escalation scheme is used for T-DM1 � T to determine the<br />
maximum tolerated dose (MTD); P is added at this MTD. Initial restrictive<br />
dose-limiting toxicity (DLT) criteria were modified to establish a more<br />
clinically relevant MTD. Results: We report interim results with T-DM1 (qw<br />
and q3w) � T(�P) using modified DLT criteria. 24 pts have been enrolled<br />
in these cohorts; median age was 53 yrs (range, 23–69)*; median number<br />
<strong>of</strong> prior systemic therapies in MBC was 7 (range, 2–15)*. See table below.<br />
Conclusions: Data support combining T-DM1 � T � P at the MTD for future<br />
clinical trials. The MTD for weekly T-DM1 � T is 2.4 mg/kg � 80 mg/m2 qw; MTD for weekly T-DM1 � T � P is 2.4 mg/kg � 80 mg/m2 qw � 840<br />
mg LD, 420 mg q3w. Updated results will be presented, including the MTD<br />
for T-DM1 q3w � Tqw� P q3w, outcomes from pts with prolonged<br />
follow-up, and duration <strong>of</strong> response from an extension trial.<br />
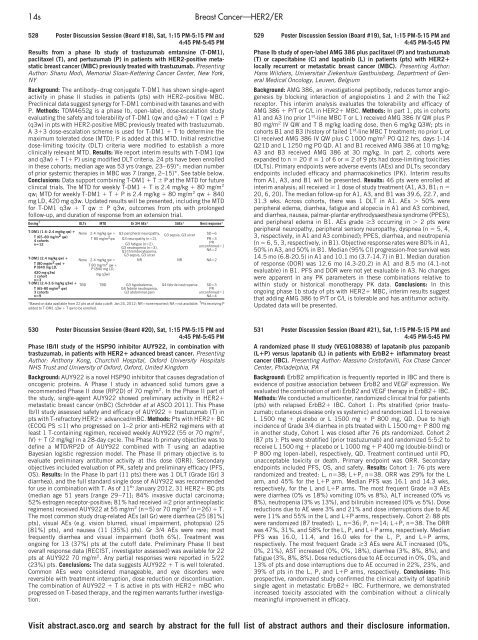
Dosing † DLTs MTD Gr 3/4 AEs* SAEs* Best response*<br />
T-DM1 (1.6–2.4 mg/kg qw) �<br />
T (65–80 mg/m 2 qw)<br />
4 cohorts<br />
n�12<br />
T-DM1 (2.4 mg/kg qw) �<br />
T (80 mg/m 2 qw) �<br />
P (840 mg LD,<br />
420 mg q3w)<br />
1 cohort<br />
n�3<br />
T-DM1 (2.4-3.6 mg/kg q3w) �<br />
T (65-80 mg/m 2 qw)<br />
3 cohorts<br />
n�9<br />
None 2.4 mg/kg qw �<br />
T80mg/m 2 qw<br />
None 2.4 mg/kg qw �<br />
T80mg/m 2 qw �<br />
P (840 mg LD,<br />
mg q3w)<br />
G3 peripheral neuropathy,<br />
G3 neuropathy (n�2),<br />
G3 fatigue (n�2),<br />
G3 neutropenia (n�3),<br />
G3 thrombocytopenia,<br />
G3 sepsis, G3 ulcer<br />
TBD TBD G3 hypokalemia,<br />
G4 febrile neutropenia,<br />
G3 abdominal pain<br />
G3 sepsis, G3 ulcer<br />
SD�6<br />
PR�3<br />
PR<br />
unconfirmed�1<br />
NA�2<br />
NR NR NA�2<br />
G4 febrile neutropenia SD�3<br />
PR<br />
unconfirmed�1<br />
NA�4<br />
*Based on data available from 22 pts as <strong>of</strong> data cut<strong>of</strong>f: Jan 24, 2012; NR�none reported; NA�not available. † Pts receiving P<br />
added to T-DM1 q3w � T qw to be enrolled.<br />
530 Poster Discussion Session (Board #20), Sat, 1:15 PM-5:15 PM and<br />
4:45 PM-5:45 PM<br />
Phase IB/II study <strong>of</strong> the HSP90 inhibitor AUY922, in combination with<br />
trastuzumab, in patients with HER2� advanced breast cancer. Presenting<br />
Author: Anthony Kong, Churchill Hospital, Oxford University Hospitals<br />
NHS Trust and University <strong>of</strong> Oxford, Oxford, United Kingdom<br />
Background: AUY922 is a novel HSP90 inhibitor that causes degradation <strong>of</strong><br />
oncogenic proteins. A Phase I study in advanced solid tumors gave a<br />
recommended Phase II dose (RP2D) <strong>of</strong> 70 mg/m2 . In the Phase II part <strong>of</strong><br />
the study, single-agent AUY922 showed preliminary activity in HER2�<br />
metastatic breast cancer (mBC) (Schröder et al ASCO 2011). This Phase<br />
Ib/II study assessed safety and efficacy <strong>of</strong> AUY922 � trastuzumab (T) in<br />
pts with T-refractory HER2� advanced/mBC. Methods: Pts with HER2� BC<br />
(ECOG PS �1) who progressed on 1–2 prior anti-HER2 regimens with at<br />
least 1 T-containing regimen, received weekly AUY922 (55 or 70 mg/m2 ,<br />
IV) � T (2 mg/kg) in a 28-day cycle. The Phase Ib primary objective was to<br />
define a MTD/RP2D <strong>of</strong> AUY922 combined with T using an adaptive<br />
Bayesian logistic regression model. The Phase II primary objective is to<br />
evaluate preliminary antitumor activity at this dose (ORR). Secondary<br />
objectives included evaluation <strong>of</strong> PK, safety and preliminary efficacy (PFS,<br />
OS). Results: In the Phase Ib part (11 pts) there was 1 DLT (Grade [Gr] 3<br />
diarrhea), and the full standard single dose <strong>of</strong> AUY922 was recommended<br />
for use in combination with T. As <strong>of</strong> 11th January 2012, 31 HER2� BC pts<br />
(median age 51 years [range 29–71]; 84% invasive ductal carcinoma;<br />
52% estrogen receptor-positive; 81% had received �2 prior antineoplastic<br />
regimens) received AUY922 at 55 mg/m2 (n�5) or 70 mg/m2 (n�26) � T.<br />
The most common study drug-related AEs (all Gr) were diarrhea (25 [81%]<br />
pts), visual AEs (e.g. vision blurred, visual impairment, photopsia) (25<br />
[81%] pts), and nausea (11 [35%] pts). Gr 3/4 AEs were rare; most<br />
frequently diarrhea and visual impairment (both 6%). Treatment was<br />
ongoing for 13 (37%) pts at the cut<strong>of</strong>f date. Preliminary Phase II best<br />
overall response data (RECIST, investigator assessed) was available for 22<br />
pts at AUY922 70 mg/m2 . Any partial responses were reported in 5/22<br />
(23%) pts. Conclusions: The data suggests AUY922 � T is well tolerated.<br />
Common AEs were considered manageable, and eye disorders were<br />
reversible with treatment interruption, dose reduction or discontinuation.<br />
The combination <strong>of</strong> AUY922 � T is active in pts with HER2� mBC who<br />
progressed on T-based therapy, and the regimen warrants further investigation.<br />
529 Poster Discussion Session (Board #19), Sat, 1:15 PM-5:15 PM and<br />
4:45 PM-5:45 PM<br />
Phase Ib study <strong>of</strong> open-label AMG 386 plus paclitaxel (P) and trastuzumab<br />
(T) or capecitabine (C) and lapatinib (L) in patients (pts) with HER2�<br />
locally recurrent or metastatic breast cancer (MBC). Presenting Author:<br />
Hans Wildiers, Universitair Ziekenhuis Gasthuisberg, Department <strong>of</strong> General<br />
Medical Oncology, Leuven, Belgium<br />
Background: AMG 386, an investigational peptibody, reduces tumor angiogenesis<br />
by blocking interaction <strong>of</strong> angiopoietins 1 and 2 with the Tie2<br />
receptor. This interim analysis evaluates the tolerability and efficacy <strong>of</strong><br />
AMG 386 � P/T or C/L in HER2� MBC. Methods: In part 1, pts in cohorts<br />
A1 and A3 (no prior 1st-line MBC T or L ) received AMG 386 IV QW plus P<br />
80 mg/m2 IV QW and T 8 mg/kg loading dose, then 6 mg/kg Q3W; pts in<br />
cohorts B1 and B3 (history <strong>of</strong> failed 1st-line MBC T treatment; no prior L or<br />
C) received AMG 386 IV QW plus C 1000 mg/m2 PO Q12 hrs, days 1-14<br />
Q21D and L 1250 mg PO QD. A1 and B1 received AMG 386 at 10 mg/kg;<br />
A3 and B3 received AMG 386 at 30 mg/kg. In part 2, cohorts were<br />
expanded to n � 20 if � 1<strong>of</strong>6or�2 <strong>of</strong> 9 pts had dose-limiting toxicities<br />
(DLTs). Primary endpoints were adverse events (AEs) and DLTs; secondary<br />
endpoints included efficacy and pharmacokinetics (PK). Interim results<br />
from A1, A3, and B1 will be presented. Results: 46 pts were enrolled at<br />
interim analysis; all received � 1 dose <strong>of</strong> study treatment (A1, A3, B1; n �<br />
20, 6, 20). The median follow-up for A1, A3, and B1 was 39.6, 22.7, and<br />
31.3 wks. Across cohorts, there was 1 DLT in A1. AEs � 50% were<br />
peripheral edema, diarrhea, fatigue and alopecia in A1 and A3 combined,<br />
and diarrhea, nausea, palmar-plantar erythrodysaesthesia syndrome (PPES),<br />
and peripheral edema in B1. AEs grade �3 occurring in � 2 pts were<br />
peripheral neuropathy, peripheral sensory neuropathy, dyspnea (n � 5, 4,<br />
3, respectively, in A1 and A3 combined); PPES, diarrhea, and neutropenia<br />
(n � 6, 5, 3, respectively, in B1). Objective response rates were 80% in A1,<br />
50% in A3, and 50% in B1. Median (95% CI) progression-free survival was<br />
14.5 mo (6.8-20.5) in A1 and 10.1 mo (3.7-14.7) in B1. Median duration<br />
<strong>of</strong> response (DOR) was 12.6 mo (4.3-20.2) in A1 and 8.5 mo (4.1-not<br />
evaluable) in B1. PFS and DOR were not yet evaluable in A3. No changes<br />
were apparent in any PK parameters in these combinations relative to<br />
within study or historical monotherapy PK data. Conclusions: In this<br />
ongoing phase 1b study <strong>of</strong> pts with HER2� MBC, interim results suggest<br />
that adding AMG 386 to P/T or C/L is tolerable and has antitumor activity.<br />
Updated data will be presented.<br />
531 Poster Discussion Session (Board #21), Sat, 1:15 PM-5:15 PM and<br />
4:45 PM-5:45 PM<br />
A randomized phase II study (VEG108838) <strong>of</strong> lapatanib plus pazopanib<br />
(L�P) versus lapatanib (L) in patients with ErbB2� inflammatory breast<br />
cancer (IBC). Presenting Author: Massimo Crist<strong>of</strong>anilli, Fox Chase Cancer<br />
Center, Philadelphia, PA<br />
Background: ErbB2 amplification is frequently reported in IBC and there is<br />
evidence <strong>of</strong> positive association between ErbB2 and VEGF expression. We<br />
evaluated the combination <strong>of</strong> anti ErbB2 and VEGF therapy in ErbB2� IBC.<br />
Methods: We conducted a multicenter, randomized clinical trial for patients<br />
(pts) with relapsed ErbB2� IBC. Cohort 1: Pts stratified (prior trastuzumab;<br />
cutaneous disease only vs systemic) and randomized 1:1 to receive<br />
L 1500 mg � placebo or L 1500 mg � P 800 mg, QD. Due to high<br />
incidence <strong>of</strong> Grade 3/4 diarrhea in pts treated with L 1500 mg� P 800 mg<br />
in another study, Cohort 1 was closed after 76 pts randomized. Cohort 2<br />
(87 pts ): Pts were stratified (prior trastuzumab) and randomized 5:5:2 to<br />
receive L 1500 mg � placebo or L 1000 mg � P 400 mg (double-blind) or<br />
P 800 mg (open-label), respectively, QD. Treatment continued until PD,<br />
unacceptable toxicity or death. Primary endpoint was ORR. Secondary<br />
endpoints included PFS, OS, and safety. Results: Cohort 1: 76 pts were<br />
randomized and treated: L, n�38; L�P, n�38. ORR was 29% for the L<br />
arm, and 45% for the L�P arm. Median PFS was 16.1 and 14.3 wks,<br />
respectively, for the L and L�P arms. The most frequent Grade �3 AEs<br />
were diarrhea (0% vs 18%) vomiting (0% vs 8%), ALT increased (0% vs<br />
8%), neutropenia (3% vs 13%), and bilirubin increased (0% vs 5%). Dose<br />
reductions due to AE were 3% and 21% and dose interruptions due to AE<br />
were 11% and 55% in the L and L�P arms, respectively. Cohort 2: 88 pts<br />
were randomized (87 treated): L, n�36; P, n�14; L�P, n�38. The ORR<br />
was 47%, 31%, and 58% for the L, P, and L�P arms, respectively. Median<br />
PFS was 16.0, 11.4, and 16.0 wks for the L, P, and L�P arms,<br />
respectively. The most frequent Grade �3 AEs were ALT increased (0%,<br />
0%, 21%), AST increased (0%, 0%, 18%), diarrhea (3%, 8%, 8%), and<br />
fatigue (3%, 8%, 8%). Dose reductions due to AE occurred in 0%, 0%, and<br />
13% <strong>of</strong> pts and dose interruptions due to AE occurred in 22%, 23%, and<br />
39% <strong>of</strong> pts in the L, P, and L�P arms, respectively. Conclusions: This<br />
prospective, randomized study confirmed the clinical activity <strong>of</strong> lapatinib<br />
single agent in metastatic ErbB2� IBC. Furthermore, we demonstrated<br />
increased toxicity associated with the combination without a clinically<br />
meaningful improvement in efficacy.<br />
Visit abstract.asco.org and search by abstract for the full list <strong>of</strong> abstract authors and their disclosure information.