Annual Meeting Proceedings Part 1 - American Society of Clinical ...
Annual Meeting Proceedings Part 1 - American Society of Clinical ...
Annual Meeting Proceedings Part 1 - American Society of Clinical ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
573 General Poster Session (Board #5H), Sat, 8:00 AM-12:00 PM<br />
In situ quantitative measurement <strong>of</strong> mRNA to predict response to trastuzumab<br />
in a cohort <strong>of</strong> metastatic breast cancer patients. Presenting Author:<br />
Maria Vassilakopoulou, Yale University, New Haven, CT<br />
Background: Trastuzumab therapy is currently selected based on assessment<br />
<strong>of</strong> HER2 by either immunohistochemistry (IHC) for protein overexpression<br />
or fluorescence in situ hybridization (FISH) to detect gene<br />
amplification. We sought to determine the predictive value <strong>of</strong> in situ<br />
quantitative measurement <strong>of</strong> mRNA on a cohort <strong>of</strong> trastuzumab-treated<br />
metastatic breast cancer patients. Methods: A tissue microarray composed<br />
<strong>of</strong> ninety metastatic breast cancers treated with various chemotherapy<br />
regimens combined with trastuzumab was constructed. HER2 intracellular<br />
domain (ICD), HER2 extracellular domain (ECD) and HER2 mRNA were<br />
assessed using the AQUA method for quantitative immun<strong>of</strong>luorescence.<br />
For HER2 protein evaluation CB11was used to measure ICD and SP3 to<br />
measure ECD <strong>of</strong> the HER2 receptor. In addition, HER2 mRNA status was<br />
assessed using the RNAscope assay ERRB2 probe according to manufacturer’s<br />
protocol modified for detection with Cy-5 Tyramide. Cytokeratin was<br />
used in order to create the tumor mask and signal was quantified within the<br />
mask. Primary endpoints included time to progression (TTP) from trastuzumab<br />
initiation and overall survival (OS) times. Statistical analysis was<br />
performed using Kaplan-Meier analysis and the Cox proportional hazard<br />
model. Results: HER mRNA was tightly correlated with ICD HER2, as<br />
measured by CB11 (r2�0.35), but not with ECD HER2 as measured by<br />
SP3 (r2�0.14). Both ICD HER2 and HER2 mRNA were predictive <strong>of</strong><br />
response to trastuzumab, but ECD was not. Multivariate analysis including<br />
age, histological grade and hormone receptor status shows the ICD to be<br />
predictive <strong>of</strong> TTP (p�0.0377). HER2 mRNA levels were significant for<br />
prediction <strong>of</strong> TTP (p�0.0344) in multivariate analysis including age and<br />
histological grade. Conclusions: The expression <strong>of</strong> ICD, as detected by<br />
CB11 and HER2 mRNA levels were significantly associated with TTP in this<br />
trastuzumab-treated metastatic cohort. The ECD, as detected by SP3 is<br />
neither predictive <strong>of</strong> response, nor tightly correlated with HER2 mRNA. In<br />
situ assessment <strong>of</strong> HER2 mRNA has the potential to identify breast cancer<br />
patients who derive benefit from trastuzumab treatment.<br />
575 General Poster Session (Board #6B), Sat, 8:00 AM-12:00 PM<br />
Fertility preservation options and the young breast cancer patient: A survey.<br />
Presenting Author: Manuela Jacobsen Junqueira, Memorial Sloan-<br />
Kettering Cancer Center, New York, NY<br />
Background: Approximately 15% <strong>of</strong> breast cancers (BC) are diagnosed in<br />
reproductive aged women. Management <strong>of</strong> the disease in this age group<br />
frequently includes chemotherapy and hormonal therapy, which can both<br />
affect fertility. Considering that age at first delivery has been steadily<br />
increasing, young women may face BC before completion <strong>of</strong> childbearing.<br />
Methods: In this prospective study, women referred to our institution for<br />
surgical treatment <strong>of</strong> BC were asked, before their first visit, to fill out a<br />
questionnaire regarding their reproductive history and fertility preservation<br />
knowledge. Eligible patients included women between the ages <strong>of</strong> 18 and<br />
45, with a newly diagnosed BC, who had not yet started treatment. Results:<br />
Sixty women were eligible with a median age <strong>of</strong> 40 (range 20-45). 98% <strong>of</strong><br />
responders (59 out <strong>of</strong> 60) had been diagnosed within the previous 2<br />
months. 78% (47/60) had a college or post-graduate degree. 80% (48/60)<br />
had been pregnant before, while 86.5% (45/52) reported having had<br />
children. 81% (47/58) were premenopausal, and only 3 patients reported<br />
not having had periods for more than 1 year. 50% <strong>of</strong> responders (30/60)<br />
declared no interest in future childbearing, 25% were definitely interested,<br />
and 25% were undecided. However, only 9% (5/57) reported having<br />
received information on fertility preservation options before the survey.<br />
Women who have been pregnant were significantly less likely to consider<br />
fertility preservation options prior to treatment (egg/embryo/ovarian tissue<br />
cryopreservation [6% vs. 50%, p�0.001]), or after treatment (egg/embryo<br />
donation, surrogacy or adoption [6% vs. 58%, p�0.0001]). Conclusions:<br />
This pilot study was designed to gather information on reproductive health<br />
<strong>of</strong> newly diagnosed young BC patients and to assess their willingness to<br />
consider various fertility preservation options before or after treatment. Our<br />
study population consisted <strong>of</strong> mostly women who had been pregnant and<br />
had children. We found that 50% <strong>of</strong> the women were unsure or wanted<br />
future children. Yet, only 9% had received information on fertility options<br />
at diagnosis. This pilot study highlights the need for education and/or<br />
intervention in fertility preservation options for young women with breast<br />
cancer.<br />
Breast Cancer—HER2/ER<br />
25s<br />
574 General Poster Session (Board #6A), Sat, 8:00 AM-12:00 PM<br />
ER� mRNA expression in ER�-negative and triple-negative breast cancers.<br />
Presenting Author: Young Choi, Yale University School <strong>of</strong> Medicine,<br />
Bridgeport, CT<br />
Background: ER� is the main prognostic and therapeutic marker in breast<br />
cancer (BC). About 30% <strong>of</strong> BC cases are negative for ER (ER�-) and do not<br />
benefit from antiestrogen therapy (TAM). We aim to study ER-beta (ER�)<br />
expression in ER�- and triple negative (TN) cancers to explore alternate<br />
pathway <strong>of</strong> treatment in this cohort. Methods: We studied 67 ER�- BC cases<br />
including 44 TN together with 74 ER� �BC cases obtained from patients<br />
aged 29 to 97 years old between 2003 and 2010. The histology included<br />
110 intraductal, 12 medullary and 19 other types. 78 cases were grade 3,<br />
52 were grade 2, and 11 were grade 1. RNA was extracted from FFPE and<br />
mRNA levels <strong>of</strong> ER� is<strong>of</strong>orm and ER� were determined by real-time<br />
quantitative reverse transcription PCR. IHC stains were done on TMA the<br />
sections for ER�, PR, Her-2, Ki-67, CK5/6 and Cyclin D1. Results: ER�<br />
is<strong>of</strong>orms were highly expressed in ER�-, TN, basal-like and HER2 type BC<br />
cases. ER�2 was the major ER� variant expressed. Ki-67 proliferating cells<br />
(�20% nuclear staining) were mostly in ER�- rather than ER�� cases<br />
(69.0% vs. 31.0%) as were cyclin D1- cells (82.2% vs. 17.8%). On the<br />
other hand, in ER�� BC, ER� mRNA expression was consistently high and<br />
upregulated, and ER�, low and down regulated, and the ratio <strong>of</strong> ER�� to<br />
ER�� ranged from 3 to 100. ER�1, 2 and 5 were co-expressed with ER� in<br />
56%, 63%, and 30% <strong>of</strong> cases, respectively. Overall, ER� mRNA levels did<br />
not show any significant correlation with age, tumor size, lymph node status<br />
and histological grades. Conclusions: ER�-dependent proliferating tumor<br />
cells may render them more sensitive to TAM, and increase the effectiveness<br />
<strong>of</strong> TAM and its metabolites in ER�- and TN cases. Increased overall<br />
survival after adjuvant TAM ER�-BC may be directly related to ER�<br />
over-expression. ER� is<strong>of</strong>orm is potential selective therapeutic target in a<br />
sub-cohort <strong>of</strong> ER�- BC. Additionally, when ER� and ER� are co-expressed,<br />
ER� appears to play a distinct role from its action in ER�- BC.<br />
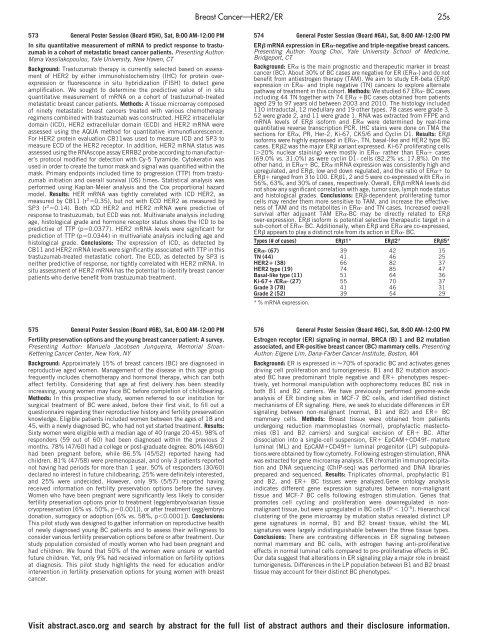
Types (# <strong>of</strong> cases) ER�1* ER�2* ER�5*<br />
ER�- (67) 39 42 15<br />
TN (44) 41 46 25<br />
HER2� (38) 66 82 37<br />
HER2 type (19) 74 85 47<br />
Basal-like type (11) 51 64 36<br />
Ki-67� /ER�- (27) 55 70 37<br />
Grade 3 (78) 41 46 31<br />
Grade 2 (52) 39 54 29<br />
* % mRNA expression.<br />
576 General Poster Session (Board #6C), Sat, 8:00 AM-12:00 PM<br />
Estrogen receptor (ER) signaling in normal, BRCA (B) 1 and B2 mutation<br />
associated, and ER-positive breast cancer (BC) mammary cells. Presenting<br />
Author: Elgene Lim, Dana-Farber Cancer Institute, Boston, MA<br />
Background: ER is expressed in �70% <strong>of</strong> sporadic BC and activates genes<br />
driving cell proliferation and tumorigenesis. B1 and B2 mutation associated<br />
BC have predominant triple negative and ER� phenotypes respectively,<br />
yet hormonal manipulation with oophorectomy reduces BC risk in<br />
both B1 and B2 carriers. We have previously performed genome-wide<br />
analysis <strong>of</strong> ER binding sites in MCF-7 BC cells, and identified distinct<br />
mechanisms <strong>of</strong> ER signaling. Here, we seek to elucidate differences in ER<br />
signaling between non-malignant (normal, B1 and B2) and ER� BC<br />
mammary cells. Methods: Breast tissue were obtained from patients<br />
undergoing reduction mammoplasties (normal), prophylactic mastectomies<br />
(B1 and B2 carriers) and surgical excision <strong>of</strong> ER� BC. After<br />
dissociation into a single-cell suspension, ER� EpCAM�CD49f- mature<br />
luminal (ML) and EpCAM�CD49f� luminal progenitor (LP) subpopulations<br />
were obtained by flow cytometry. Following estrogen stimulation, RNA<br />
was extracted for gene microarray analysis. ER chromatin immunoprecipitation<br />
and DNA sequencing (ChIP-seq) was performed and DNA libraries<br />
prepared and sequenced. Results: Triplicates <strong>of</strong>normal, prophylactic B1<br />
and B2, and ER� BC tissues were analyzed.Gene ontology analysis<br />
indicates different gene expression signatures between non-malignant<br />
tissue and MCF-7 BC cells following estrogen stimulation. Genes that<br />
promotes cell cycling and proliferation were downregulated in nonmalignant<br />
tissue, but were upregulated in BC cells (P � 10-5 ). Hierarchical<br />
clustering <strong>of</strong> the gene microarray by mutation status revealed distinct LP<br />
gene signatures in normal, B1 and B2 breast tissue, whilst the ML<br />
signatures were largely indistinguishable between the three tissue types.<br />
Conclusions: There are contrasting differences in ER signaling between<br />
normal mammary and BC cells, with estrogen having anti-proliferative<br />
effects in normal luminal cells compared to pro-proliferative effects in BC.<br />
Our data suggest that alterations in ER signaling play a major role in breast<br />
tumorigenesis. Differences in the LP population between B1 and B2 breast<br />
tissue may account for their distinct BC phenotypes.<br />
Visit abstract.asco.org and search by abstract for the full list <strong>of</strong> abstract authors and their disclosure information.