- Page 1 and 2:
Antibiotikaprofylax vid kirurgiska
- Page 3:
Antibiotikaprofylax vid kirurgiska
- Page 6 and 7:
3. Antibiotikaprofylax - praxis 57
- Page 8 and 9:
Har antibiotikaimpregnerade grafter
- Page 10 and 11:
Resultat av litteratursökningen oc
- Page 12 and 13:
4.11 Sluten inläggning av thoraxdr
- Page 14 and 15:
5. Infektionsprofylax utan antibiot
- Page 17 and 18:
SBU:s sammanfattning och slutsatser
- Page 19 and 20:
Bakgrund och syfte Antibiotika i pr
- Page 21 and 22:
arhet. Kvalitetsgranskningen av de
- Page 23 and 24:
Det vetenskapliga underlaget saknas
- Page 25 and 26:
tagning av livmoder (måttligt star
- Page 27 and 28:
Bröstcancerkirurgi • Vid bröstc
- Page 29 and 30:
sårinfektion, empyem (varansamling
- Page 31 and 32:
• Antibiotikaprofylax vid öppen
- Page 33 and 34:
Infektiös endokardit Infektiös en
- Page 35:
• Endovaskulära ingrepp, speciel
- Page 38 and 39:
1.2 Avgränsningar Projektet omfatt
- Page 40 and 41:
Tabell 1.1 Effektmått förutom pos
- Page 42 and 43:
Tabell 1.2 fortsättning Antal bakt
- Page 44 and 45:
Proteinbindning Många antibiotika
- Page 46 and 47:
Till allmänna faktorer räknas ock
- Page 49 and 50:
2. Metodik för systematisk littera
- Page 51 and 52:
Figur 2.1 Granskningsprocessen. Fas
- Page 53 and 54:
Evidensstyrkan graderades i fyra ni
- Page 55 and 56:
3. Antibiotikaprofylax - praxis KAP
- Page 57 and 58:
3.1 Praxisundersökning om användn
- Page 59 and 60:
100 90 80 70 Procent Ja-svar 60 50
- Page 61 and 62:
De 37 kliniker som uppgav att de re
- Page 63 and 64:
Urologi Samtliga 13 kliniker som be
- Page 65 and 66:
Tabell 3.1.2 Finns skriftliga anvis
- Page 67 and 68:
72 antibiotikaprofylax vid kirurgis
- Page 69 and 70:
esistens). STRAMA-gruppen har delat
- Page 71 and 72:
Tabell 3.2.2 fortsättning Preparat
- Page 73 and 74:
Tabell 3.2.2 fortsättning Preparat
- Page 76 and 77:
4. Den systematiska litteraturöver
- Page 78 and 79:
4.1 Antibiotikaprofylax vid gastroi
- Page 80 and 81:
• Blindtarmsinflammation: Antibio
- Page 82 and 83:
Frågeställningar • Vilken typ a
- Page 84 and 85:
Weber och medarbetare publicerade 2
- Page 86 and 87:
Accidentell perforation under opera
- Page 88 and 89:
Ventrikelkirurgi (Tabell 4.1.10) Ba
- Page 90 and 91:
Det finns idag inga RCT av antibiot
- Page 92 and 93:
Table 4.1.3 Timing. Author Year Ref
- Page 94 and 95:
Table 4.1.4 continued Author Year R
- Page 96 and 97:
Table 4.1.4 continued Author Year R
- Page 98 and 99:
Table 4.1.5 continued Author Year R
- Page 100 and 101:
Table 4.1.5 continued Author Year R
- Page 102 and 103:
Table 4.1.6 ERCP. Author Year Refer
- Page 104 and 105:
Table 4.1.9 Oesophagus. Author Year
- Page 106 and 107:
Table 4.1.10 continued Author Year
- Page 108 and 109:
Table 4.1.10 continued Author Year
- Page 110 and 111:
Table 4.1.12 Hernia repair. Author
- Page 112 and 113:
Table 4.1.12 continued Author Year
- Page 114 and 115:
Table 4.1.13 Appendectomy. Author Y
- Page 116 and 117:
Referenser 1. Bai Y, Gao F, Gao J,
- Page 118 and 119:
laxis during elective upper gastroi
- Page 120 and 121:
57. Sanchez-Manuel FJ, Lozano Garci
- Page 122 and 123:
152 antibiotikaprofylax vid kirurgi
- Page 124 and 125:
• De flesta studier har jämfört
- Page 126 and 127:
Frågeställningar • Vilken antib
- Page 128 and 129:
(RR = 0,41; 95 procent KI = 0,23-0,
- Page 130 and 131:
Diskussion Idag använder 67 procen
- Page 132 and 133:
Table 4.2.2 Elective colorectal sur
- Page 134 and 135:
Table 4.2.2 continued Author Year R
- Page 136 and 137:
Table 4.2.2 continued Author Year R
- Page 138 and 139:
Table 4.2.2 continued Author Year R
- Page 140 and 141:
Table 4.2.2 continued Author Year R
- Page 142 and 143:
Table 4.2.3 Elective colorectal sur
- Page 144 and 145:
mycin as antibiotic prophylaxis in
- Page 146 and 147:
Bakgrund Infektioner hos patienter
- Page 148 and 149:
Beskrivning av studier och resultat
- Page 150 and 151:
Table 4.3.2 Vascular surgery. Autho
- Page 152 and 153:
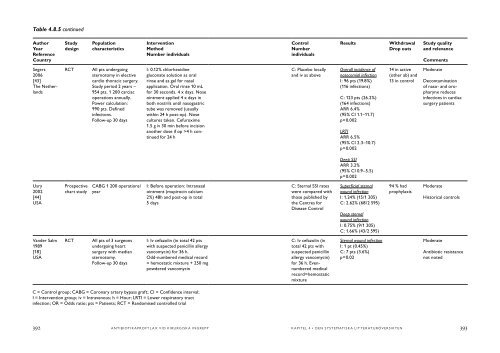
Table 4.3.2 continued Author Year R
- Page 154 and 155:
Table 4.3.3 Low study quality and r
- Page 156 and 157:
Referenser 1. Christenson JT, Eklof
- Page 158 and 159:
a randomized, prospective trial. So
- Page 160 and 161:
Elektivt sectio (generellt) • Ant
- Page 162 and 163:
Transcervikala intrauterina ingrepp
- Page 164 and 165:
Vid bakteriell vaginos som kan vara
- Page 166 and 167:
Beskrivning av studier och resultat
- Page 168 and 169:
endometrit (1 procent vs 5 procent)
- Page 170 and 171:
[4]. Inga av de förhållandevis f
- Page 172 and 173:
frekvens av infektioner efter profy
- Page 174 and 175:
Det finns inga data som visar att f
- Page 176 and 177:
Sterilisering I en stor studie frå
- Page 178 and 179:
Table 4.4.2 Caesarean section, anti
- Page 180 and 181:
Table 4.4.3 Caesarean section, comp
- Page 182 and 183:
Table 4.4.5 Caesarean section, mult
- Page 184 and 185:
Table 4.4.6 continued Author Year R
- Page 186 and 187:
Table 4.4.8 Hysterectomy, antibioti
- Page 188 and 189:
Table 4.4.8 continued Author Year R
- Page 190 and 191:
Table 4.4.10 Hysterectomy, duration
- Page 192 and 193:
Table 4.4.12 continued Author Year
- Page 194 and 195:
Table 4.4.14 Intrauterine contracep
- Page 196 and 197:
Table 4.4.16 continued Author Year
- Page 198 and 199:
Table 4.4.16 continued Author Year
- Page 200 and 201:
Table 4.4.16 continued Author Year
- Page 202 and 203:
15. Sullivan SA, Smith T, Chang E,
- Page 204 and 205:
hysterectomy. Clin Infect Dis 1995;
- Page 206 and 207:
urethropexy. Journal of Pelvic Medi
- Page 208 and 209:
97. Mangioni C, Bianchi L, Bolis PF
- Page 210 and 211:
4.5 Antibiotikaprofylax vid ortoped
- Page 212 and 213:
inte sällan i kronisk form. Insät
- Page 214 and 215:
Inklusionskriterier Enbart prospekt
- Page 216 and 217:
och medarbetare från år 1987 [9]
- Page 218 and 219:
(från 1998) samtidigt som man helt
- Page 220 and 221:
KAPITEL 4 • den systematiska litt
- Page 222 and 223:
Thomsen 1990 [44] Denmark RCT, open
- Page 224 and 225:
Table 4.5.3 Closed fractures; durat
- Page 226 and 227:
Table 4.5.3 continued Author Year R
- Page 228 and 229:
Table 4.5.5 Studies comparing diffe
- Page 230 and 231:
Table 4.5.5 continued Author Year R
- Page 232 and 233:
Table 4.5.7 Prosthesis, different d
- Page 234 and 235:
Table 4.5.7 continued Author Year R
- Page 236 and 237:
Table 4.5.9 Prosthesis and antibiot
- Page 238 and 239:
Table 4.5.11 Low study quality and
- Page 240 and 241:
Table 4.5.11 continued Author Year
- Page 242 and 243:
prophylaxis in trochanteric hip fra
- Page 244 and 245:
45. Nungu KS, Olerud C, Rehnberg L,
- Page 246 and 247: 324 antibiotikaprofylax vid kirurgi
- Page 248 and 249: Det är oklart om antibiotikaprofyl
- Page 250 and 251: Resultat av litteratursökningen oc
- Page 252 and 253: Två artiklar med medelhög kvalite
- Page 254 and 255: Övrig plastikkirurgi Två artiklar
- Page 256 and 257: Table 4.6.2 Skin surgery. Author Ye
- Page 258 and 259: Table 4.6.3 Breast surgery. Author
- Page 260 and 261: Table 4.6.4 Abdominoplasty. Author
- Page 262 and 263: Referenser 1. Amland PF, Andenaes K
- Page 264 and 265: 348 antibiotikaprofylax vid kirurgi
- Page 266 and 267: I en del situationer görs en omede
- Page 268 and 269: Bröstcancerbehandling har genomgå
- Page 270 and 271: Table 4.7.2 Breast cancer operation
- Page 272 and 273: 4.8 Antibiotikaprofylax vid hjärtk
- Page 274 and 275: Det finns flera för hjärtkirurgi
- Page 276 and 277: Bakteriologi/bakteriologisk miljö
- Page 278 and 279: Alternativ till antibiotikaprofylax
- Page 280 and 281: Preparatval (Tabell 4.8.3) Det stor
- Page 282 and 283: av dessa studier för få patienter
- Page 284 and 285: studier av effektivitet och resiste
- Page 286 and 287: Table 4.8.2 continued Author Year R
- Page 288 and 289: Table 4.8.3 Choice of antibiotics.
- Page 290 and 291: Table 4.8.3 continued Author Year R
- Page 292 and 293: Table 4.8.4 continued Author Year R
- Page 294 and 295: Table 4.8.5 Alternatives to intrave
- Page 298 and 299: 14. Kadurugamuwa JL, Beveridge TJ.
- Page 300 and 301: infections after cardiac surgery: a
- Page 302 and 303: 4.9 Antibiotikaprofylax vid implant
- Page 304 and 305: Resultat av litteratursökningen oc
- Page 306 and 307: KAPITEL 4 • den systematiska litt
- Page 308 and 309: Table 4.9.2 continued Author Year R
- Page 310 and 311: 4.10 Antibiotikaprofylax vid allmä
- Page 312 and 313: tionstekniken har även ändrats se
- Page 314 and 315: penicillin och ett dygns cefuroxim
- Page 316 and 317: etiologi som uppkomstmekanism. Dett
- Page 318 and 319: Table 4.10.2 continued Author Year
- Page 320 and 321: Referenser 1. Aznar R, Mateu M, Mir
- Page 322 and 323: Tabell 4.11.1 Antibiotikaprofylax j
- Page 324 and 325: medelhög kvalitet. Fyra av de ing
- Page 326 and 327: av hemothorax har vidare angivits s
- Page 328 and 329: Table 4.11.1 Penetrating injuries o
- Page 330 and 331: Referenser 1. Fallon WF, Jr, Wears
- Page 332 and 333: • Stötvågsbehandling av njurste
- Page 334 and 335: ersatt den öppna kirurgin för van
- Page 336 and 337: Beskrivning av studier och resultat
- Page 338 and 339: är fastställd. I en undersökning
- Page 340 and 341: 0 och 5,1 procent hos patienter uta
- Page 342 and 343: Här följer några exempel: Abdomi
- Page 344 and 345: infektion. Det finns i de redovisad
- Page 346 and 347:
Table 4.12.3 Cystoscopy. Author Yea
- Page 348 and 349:
Table 4.12.4 Transrectal prostatic
- Page 350 and 351:
Table 4.12.4 continued Author Year
- Page 352 and 353:
Table 4.12.4 continued Author Year
- Page 354 and 355:
Table 4.12.6 Transurethral resectio
- Page 356 and 357:
Table 4.12.8 Extracorporeal Shockwa
- Page 358 and 359:
Table 4.12.8 continued Author Year
- Page 360 and 361:
Table 4.12.10 Percutaneous nephroli
- Page 362 and 363:
Table 4.12.12 Low study quality and
- Page 364 and 365:
Referenser 1. Berry A, Barratt A. P
- Page 366 and 367:
cin and chloramphenicol. Int Braz J
- Page 368 and 369:
urine culture and sensitivity are b
- Page 370 and 371:
490 antibiotikaprofylax vid kirurgi
- Page 372 and 373:
• Det vetenskapliga underlaget f
- Page 374 and 375:
Kirurgiska ingrepp inom öron-näsa
- Page 376 and 377:
ständiga artiklarna resulterade i
- Page 378 and 379:
Cancerkirurgi (Tabell 4.13.5) En RC
- Page 380 and 381:
Sinuskirurgi (Tabell 4.13.8) En ran
- Page 382 and 383:
Typ av antibiotika och dos varierad
- Page 384 and 385:
Table 4.13.3 Tonsillectomy. Author
- Page 386 and 387:
Table 4.13.5 Cancer. Author Year Re
- Page 388 and 389:
Table 4.13.5 continued Author Year
- Page 390 and 391:
Table 4.13.6 Rhinosurgery. Author Y
- Page 392 and 393:
Table 4.13.9 Low study quality and
- Page 394 and 395:
and neck oncologic surgery. Ann Oto
- Page 396 and 397:
524 antibiotikaprofylax vid kirurgi
- Page 398 and 399:
• Det vetenskapliga underlaget ä
- Page 400 and 401:
Frågeställningar • Vid vilka ki
- Page 402 and 403:
Anomalikirurgi (Tabell 4.14.3) Anom
- Page 404 and 405:
Övriga kirurgiska ingrepp i käkar
- Page 406 and 407:
utförde Lockhart och medarbetare (
- Page 408 and 409:
Table 4.14.2 Third molar surgery. A
- Page 410 and 411:
Table 4.14.3 Orthognatic surgery. A
- Page 412 and 413:
Table 4.14.4 Implant surgery. Autho
- Page 414 and 415:
Table 4.14.6 Other dentoalveolar su
- Page 416 and 417:
Table 4.14.8 Low quality and releva
- Page 418 and 419:
Table 4.14.8 continued Author Year
- Page 420 and 421:
Referenser 1. Esposito M, Grusovin
- Page 422 and 423:
preoperative single-dose clindamyci
- Page 424 and 425:
560 antibiotikaprofylax vid kirurgi
- Page 426 and 427:
• Sjukvården får kostnader för
- Page 428 and 429:
358 (p
- Page 430 and 431:
Table 4.15.1 Antibiotic prophylaxis
- Page 432 and 433:
Table 4.15.2 Antibiotic prophylaxis
- Page 434 and 435:
5. Infektionsprofylax utan antibiot
- Page 436 and 437:
frekvensen postoperativa sårinfekt
- Page 438 and 439:
6. Etiska aspekter Infektioner rela
- Page 440 and 441:
komplikation roll. Vissa komplikati
- Page 442 and 443:
• Hur garanterades bästa möjlig
- Page 444 and 445:
Etisk analys med hjälp av aktörsm
- Page 446:
Referens 1. Hermerén G. Kunskapens
- Page 449 and 450:
Granskningen av hälsoekonomisk lit
- Page 451 and 452:
Distala Duodenum E Coli ”Efficien
- Page 453 and 454:
KNS Kolecystektomi Kolecystit Koled
- Page 455 and 456:
Preoperativa Protesendokoardit Pseu
- Page 458 and 459:
9. Projektgrupp, externa granskare,
- Page 460 and 461:
Adjungerade Mats Bergström Läkare
- Page 462 and 463:
Principal Investigator för Sepsiss
- Page 464 and 465:
Därutöver konsult/rådgivningsarv
- Page 466 and 467:
Rapporter publicerade av SBU Gula r
- Page 468:
Självtestning och egenvård vid an