ELECTRONIC POSTER - ismrm
ELECTRONIC POSTER - ismrm
ELECTRONIC POSTER - ismrm
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
elaxation provided the intracellular T1 and intracellular fraction, measures of β cell labeling. Increased intracellular T1 and lower<br />
intracellular fraction in nifedipine-treated mice confirmed Mn2+ enters β cells through Ca2+ channels. The timecourse of intracellular<br />
T1 and fraction in normal mice revealed 3 phases of Mn2+ kinetics: 1) labeling β cells, 2). washout from β cells, 3). nonspecific<br />
labeling of other cells.<br />
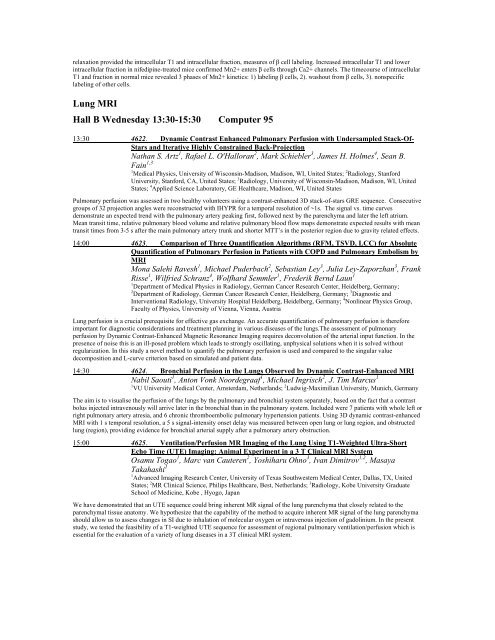
Lung MRI<br />
Hall B Wednesday 13:30-15:30 Computer 95<br />
13:30 4622. Dynamic Contrast Enhanced Pulmonary Perfusion with Undersampled Stack-Of-<br />
Stars and Iterative Highly Constrained Back-Projection<br />
Nathan S. Artz 1 , Rafael L. O'Halloran 2 , Mark Schiebler 3 , James H. Holmes 4 , Sean B.<br />
Fain 1,3<br />
1 Medical Physics, University of Wisconsin-Madison, Madison, WI, United States; 2 Radiology, Stanford<br />
University, Stanford, CA, United States; 3 Radiology, University of Wisconsin-Madison, Madison, WI, United<br />
States; 4 Applied Science Laboratory, GE Healthcare, Madison, WI, United States<br />
Pulmonary perfusion was assessed in two healthy volunteers using a contrast-enhanced 3D stack-of-stars GRE sequence. Consecutive<br />
groups of 32 projection angles were reconstructed with IHYPR for a temporal resolution of ~1s. The signal vs. time curves<br />
demonstrate an expected trend with the pulmonary artery peaking first, followed next by the parenchyma and later the left atrium.<br />
Mean transit time, relative pulmonary blood volume and relative pulmonary blood flow maps demonstrate expected results with mean<br />
transit times from 3-5 s after the main pulmonary artery trunk and shorter MTT’s in the posterior region due to gravity related effects.<br />
14:00 4623. Comparison of Three Quantification Algorithms (RFM, TSVD, LCC) for Absolute<br />
Quantification of Pulmonary Perfusion in Patients with COPD and Pulmonary Embolism by<br />
MRI<br />
Mona Salehi Ravesh 1 , Michael Puderbach 2 , Sebastian Ley 3 , Julia Ley-Zaporzhan 3 , Frank<br />
Risse 1 , Wilfried Schranz 4 , Wolfhard Semmler 1 , Frederik Bernd Laun 1<br />
1 Department of Medical Physics in Radiology, German Cancer Research Center, Heidelberg, Germany;<br />
2 Department of Radiology, German Cancer Research Center, Heidelberg, Germany; 3 Diagnostic and<br />
Interventional Radiology, University Hospital Heidelberg, Heidelberg, Germany; 4 Nonlinear Physics Group,<br />
Faculty of Physics, University of Vienna, Vienna, Austria<br />
Lung perfusion is a crucial prerequisite for effective gas exchange. An accurate quantification of pulmonary perfusion is therefore<br />
important for diagnostic considerations and treatment planning in various diseases of the lungs.The assessment of pulmonary<br />
perfusion by Dynamic Contrast-Enhanced Magnetic Resonance Imaging requires deconvolution of the arterial input function. In the<br />
presence of noise this is an ill-posed problem which leads to strongly oscillating, unphysical solutions when it is solved without<br />
regularization. In this study a novel method to quantify the pulmonary perfusion is used and compared to the singular value<br />
decomposition and L-curve criterion based on simulated and patient data.<br />
14:30 4624. Bronchial Perfusion in the Lungs Observed by Dynamic Contrast-Enhanced MRI<br />
Nabil Saouti 1 , Anton Vonk Noordegraaf 1 , Michael Ingrisch 2 , J. Tim Marcus 1<br />
1 VU University Medical Center, Amsterdam, Netherlands; 2 Ludwig-Maximilian University, Munich, Germany<br />
The aim is to visualise the perfusion of the lungs by the pulmonary and bronchial system separately, based on the fact that a contrast<br />
bolus injected intravenously will arrive later in the bronchial than in the pulmonary system. Included were 7 patients with whole left or<br />
right pulmonary artery atresia, and 6 chronic thromboembolic pulmonary hypertension patients. Using 3D dynamic contrast-enhanced<br />
MRI with 1 s temporal resolution, a 5 s signal-intensity onset delay was measured between open lung or lung region, and obstructed<br />
lung (region), providing evidence for bronchial arterial supply after a pulmonary artery obstruction.<br />
15:00 4625. Ventilation/Perfusion MR Imaging of the Lung Using T1-Weighted Ultra-Short<br />
Echo Time (UTE) Imaging: Animal Experiment in a 3 T Clinical MRI System<br />
Osamu Togao 1 , Marc van Cauteren 2 , Yoshiharu Ohno 3 , Ivan Dimitrov 1,2 , Masaya<br />
Takahashi 1<br />
1 Advanced Imaging Research Center, University of Texas Southwestern Medical Center, Dallas, TX, United<br />
States; 2 MR Clinical Science, Philips Healthcare, Best, Netherlands; 3 Radiology, Kobe University Graduate<br />
School of Medicine, Kobe , Hyogo, Japan<br />
We have demonstrated that an UTE sequence could bring inherent MR signal of the lung parenchyma that closely related to the<br />
parenchymal tissue anatomy. We hypothesize that the capability of the method to acquire inherent MR signal of the lung parenchyma<br />
should allow us to assess changes in SI due to inhalation of molecular oxygen or intravenous injection of gadolinium. In the present<br />
study, we tested the feasibility of a T1-weighted UTE sequence for assessment of regional pulmonary ventilation/perfusion which is<br />
essential for the evaluation of a variety of lung diseases in a 3T clinical MRI system.